What is Heel Pain?
Heel pain can affect people across different age groups and lifestyles, often starting off mildly before becoming more noticeable in daily routines. For some, it might appear after long hours on their feet. For others, it develops without a clear reason but continues to linger with time.
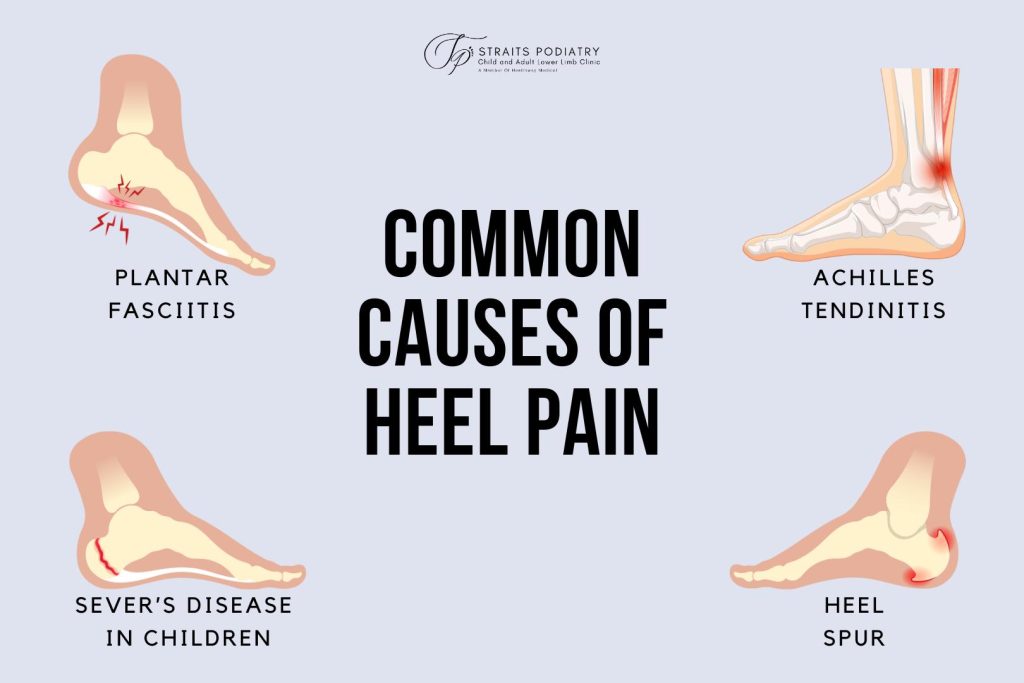
The discomfort might be linked to a range of factors, including certain conditions and everyday habits. Plantar fasciitis, heel spurs, and stress on the Achilles tendon are some of the possible sources of heel pain. At the same time, prolonged standing, walking on hard floors, or wearing unsupportive footwear might increase the pressure on your heels. Even walking barefoot at home can contribute to discomfort over time.
Since heel pain can stem from different causes, recognising what might be contributing to yours is a practical first step. In the next section, we look at the types of heel pain and how they might present.
Types of Heel Pain
Heel pain can arise from a range of underlying conditions, each with its own set of symptoms and aggravating factors. Recognising the possible type of heel pain you are experiencing can help guide you toward more targeted support and preventive care.
Here are several known causes of heel pain:
- Achilles Tendonitis: This refers to inflammation of the Achilles tendon, which connects the calf muscle to the heel bone. It often develops due to overuse or repetitive strain, especially in active individuals. The pain usually appears at the back of the heel and might worsen with activity or after periods of rest.
- Cracked Heels: While not a structural cause of heel pain, cracked heels can still cause significant discomfort, especially when the skin becomes dry and begins to split. Walking or standing for long periods can make the pain worse, particularly if the skin around the heel is already inflamed or bleeding.
- Haglund’s Deformity: This condition involves a bony enlargement on the back of the heel. It is commonly triggered by irritation from stiff or high-backed shoes. Symptoms might include swelling and tenderness, particularly when wearing enclosed footwear. It is sometimes referred to as “pump bump”.
- Heel Bursitis: Bursitis occurs when the fluid-filled sacs around the heel become inflamed. There are several types, depending on the affected area:
- Retrocalcaneal Bursitis: Involves inflammation between the Achilles tendon and heel bone. This might develop from repeated motion or pressure from tight footwear.
- Subcutaneous Calcaneal Bursitis: This type of bursitis affects the area between the skin and the Achilles tendon. It is often caused by direct shoe pressure.
- Sub Achilles Bursitis: This type occurs beneath the Achilles tendon and might cause pain or tenderness at the back of the heel, especially with continued use or pressure.
- Heel Spurs: These are calcium deposits that develop into bony projections on the underside of the heel bone. While often associated with plantar fasciitis, they do not always cause symptoms. When heel pain does occur, it tends to be sharp and noticeable during the first steps after rest.
- Plantar Fasciitis: One of the more common sources of heel pain, plantar fasciitis involves irritation of the thick band of tissue that supports the arch of the foot. Pain is typically felt under the heel and is most intense in the morning or after long periods of sitting or standing.
- Sever’s Disease: This is a heel condition that affects growing children, especially those involved in sports. It occurs when the growth plate in the heel becomes irritated. The pain often flares up with high-impact activity such as jumping or running.
- Stress Fractures: Stress fractures are tiny cracks in the calcaneus (heel bone), usually caused by repeated impact or overuse. They tend to develop gradually and lead to persistent heel pain during weight-bearing activities. This is more common among runners and individuals with increased physical demands.
- Tarsal Tunnel Syndrome: This condition results from compression of the posterior tibial nerve, which runs along the inside of the ankle and into the foot. It might cause heel pain along with tingling or numbness, and symptoms can sometimes radiate across the sole of the foot.
Need Help? See A Podiatrist Today
Symptoms of Heel Pain
Depending on the underlying cause, heel pain might feel sharp, dull, radiating, or even tingling. For some, the pain begins suddenly. For others, it builds gradually over time. Understanding how your heel pain presents can help narrow down possible causes and guide your next steps.
Here are some of the more commonly reported symptoms:
- Aching Pain: A constant, low-grade ache that worsens with prolonged standing or walking might be linked to long-term stress on the heel structures. This type of heel pain can sometimes spread toward the arch of the foot.
- Bruising/Localised Pain: Pain that is focused on a specific area of the heel and worsens with weight-bearing activity might be accompanied by bruising. These symptoms often develop gradually and might suggest repeated impact or overuse.
- Burning/Tingling Sensation: A burning or tingling feeling that moves from the heel toward the foot may suggest nerve compression. This symptom can become more noticeable during activity and might occur alongside numbness.
- Cold Sensation/Numbness: A feeling of cold or numbness in the heel, combined with ongoing pain, might be related to reduced blood flow. This is more likely in people with underlying metabolic issues or vascular conditions.
- Menopausal Joint Pain: During menopause, hormonal shifts can lead to joint stiffness and increased heel pain. Weight changes during this period might also place added pressure on the heel, making symptoms more noticeable over time.
- Morning Stiffness and Joint Pain: In some cases, heel pain is accompanied by stiffness and swelling in other joints, especially in the morning. These symptoms may be part of a broader inflammatory condition affecting more than just the heel.
- Pain Triggered by Activity: In children, heel pain that worsens during running or jumping may be linked to strain near the growth plate. The pain usually settles with rest and is most noticeable at the back or bottom of the heel.
- Radiating Pain: Some types of heel pain extend beyond the heel itself, radiating toward the arch or toes. This might occur with walking or standing and can signal pressure on nearby nerves or soft tissues.
- Redness, Heat, and Sudden Pain: In certain cases, heel pain appears suddenly and is accompanied by redness, heat, or swelling. This could point to a flare-up of joint inflammation, particularly in conditions where uric acid buildup (gout) affects the heel.
- Sharp Pain: A sharp, stabbing sensation under the heel is often most noticeable when taking the first steps in the morning. This pain might ease slightly with movement but can return after prolonged standing or walking. It is frequently linked to strain on the plantar fascia.
- Stiffness and Limited Mobility: Stiffness in the heel or ankle, especially after rest, can make it difficult to flex or extend the foot fully. This reduced mobility is commonly noticed during the first steps of the day or after sitting for long periods.
- Swelling and Tenderness: Some people experience swelling around the back or bottom of the heel, often paired with tenderness when pressure is applied. These symptoms might worsen with walking or tight footwear and are sometimes related to irritation in the tendon or surrounding tissues.
Common Causes of Heel Pain
Heel pain can begin subtly or appear after specific activity. In many cases, it develops due to a combination of lifestyle habits and physical stress. While some causes are related to movement, others involve health conditions that affect how the heel responds to pressure and weight. Understanding these contributing factors can help you take early steps to reduce strain and protect your feet.
Here are some of the more frequently reported causes of heel pain:
- Abnormal Walking Style: The way you walk can influence how weight is transferred through your foot. If your feet roll inward too much (overpronation), added tension can build along the heel and ankle. Over time, this might increase the likelihood of plantar fasciitis or tendon-related pain.
- Age-related Changes: As you age, the natural fat pad under the heel tends to thin out. With less padding, the heel becomes more sensitive to everyday forces such as walking or standing. This reduced cushioning makes the heel more vulnerable to pain and inflammation.
- Bursitis: Bursae are small fluid-filled sacs that help reduce friction between tissues. When they become irritated, especially near the heel bone, movement or pressure may trigger heel pain. This is often the case with retrocalcaneal bursitis, which affects the area behind the Achilles tendon.
- Growth Spurts in Children: During growth phases, especially in active children, inflammation of the heel’s growth plate might occur. This leads to pain that worsens during physical activity and improves with rest. It typically appears at the back or underside of the heel.
- Heel Trauma: Small injuries to the heel might build up over time. These often go unnoticed at first but can eventually lead to inflammation, swelling, or bruising. In some cases, repeated microtrauma might result in small fractures that cause pain during daily activity.
- Improper Footwear: Shoes that lack proper cushioning or arch support can affect how pressure is distributed across your foot. When the heel is left unsupported, stress builds gradually. This might contribute to plantar fasciitis or irritation in the heel’s support structures over time.
- Overuse and Repetitive Stress: Activities that involve repeated impact on your feet such as running, jumping, or standing for long periods might place excess strain on the heel. Without enough recovery time, this can affect soft tissue or bone and lead to conditions like plantar fasciitis or stress fractures.
- Standing/Moving on Hard Surfaces: Spending long hours on hard surfaces, especially without supportive footwear, can affect the soft tissue beneath the heel. The repeated impact from standing or walking might lead to irritation, inflammation, or soreness in the heel area.
- Underlying Medical Conditions: Certain long-term conditions can contribute to heel pain. For example, rheumatoid arthritis might cause joint swelling and stiffness, while diabetes can affect circulation and nerve sensitivity. These changes might alter how the heel responds to movement and weight.
- Weight Gain or Obesity: Carrying additional weight places more pressure on the heels. This can aggravate existing soreness and increase the risk of developing heel pain with walking or standing. The added stress might also slow down healing if an injury is already present.

Managing and Preventing Heel Pain
When heel pain starts affecting your daily movement, even simple tasks like walking or standing can become uncomfortable. Fortunately, there are ways to ease the strain. While the right approach depends on the cause, many cases improve with consistent care and a few supportive habits.
Here are some commonly used strategies to reduce heel pain and support recovery:
- Anti-inflammatory Medication: Nonsteroidal Anti-inflammatory Drugs (NSAIDs) might be recommended to reduce swelling and ease discomfort. These are typically used for short-term relief.
- Custom Shoe Insoles: Inserts placed inside your shoes can redistribute pressure across the foot and provide added cushioning. Custom orthotics are sometimes recommended for ongoing support if foot structure or gait contributes to the pain.
- Rest and Ice: Taking breaks from weight-bearing activity can help ease irritation, especially when heel pain follows overuse. Applying a cold compress for short periods might also reduce inflammation and soothe sore tissue.
- Stretch and Strengthen: Stretching the calves and the band of tissue beneath the foot might improve flexibility and reduce tension at the heel. Strengthening the surrounding muscles can also provide better support for daily movement.
- Shockwave or Magnetotransduction Therapy: For cases that do not improve with rest and stretching, technologies like ESWT or EMTT might be considered. These approaches are designed to encourage tissue repair and reduce discomfort over time.
Once the situation improves, it’s important to take steps to prevent heel pain from recurring. Small changes in habits, movement, and choice of footwear can help reduce strain to the heel throughout the day:
- Avoid Walking Barefoot on Hard Surfaces: At home, opt for supportive slippers or shoes with soft soles instead of walking barefoot on hard surfaces. This helps absorb impact and reduce unnecessary stress.
- Maintain a Healthy Weight: Maintaining a healthy weight range would help reduce the load placed on your heels. This also lowers the risk of overuse injuries.
- Rest Your Feet: If your daily routine involves standing or walking for extended periods, take moments to sit, stretch or shift your weight. These short breaks can go a long way in preventing overuse.
- Warm Up Before Any Activity: Prepare your body for movement with gentle stretches and low-intensity activity. This helps reduce the risk of sudden strain during more vigorous exercise.
- Wear Shoes that Fit Properly: Choose shoes with adequate cushioning and arch support. Avoid footwear with thin soles, high heels, or worn-out midsoles that can increase pressure on the heel.

Get Support for Heel Pain at Straits Podiatry
Heel pain can develop gradually or appear after specific activity, making everyday movement feel more tiring than usual. Whether it shows up during your first steps in the morning or builds after a long day on your feet, it’s often a sign that your heel might be under more stress than it can comfortably manage.
At Straits Podiatry, we help identify the factors contributing to that stress and offer guidance on care options that support mobility and provide comfort. If heel pain has been affecting your daily life, contact us today to speak with our team or schedule a consultation for a detailed assessment
Share this with someone you know
Frequently Asked Questions on heel pain
What is heel pain?
Heel pain is discomfort at the back or underside of the heel, typically triggered by repeated stress. Because the heel bone (calcaneus) absorbs impact during walking, running, and prolonged standing, excess pressure can build up. As this impact accumulates, it strains nearby tissues such as the plantar fascia and the Achilles tendon. When these structures become irritated, pain might manifest during movement and sometimes even at rest. If the strain persists without adequate support, heel pain can alter your gait and eventually limit daily activity.
What causes heel pain?
Although heel pain often begins with repeated stress, it can also be shaped by the way your feet move and the alignment of your body. For instance, flat feet, high arches, or an uneven gait can gradually place extra strain on the heel. As this imbalance persists, conditions such as plantar fasciitis or heel spurs might develop in response. In some cases, inflammatory conditions like rheumatoid arthritis or gout might also play a role, especially when joint inflammation or uric acid crystal buildup affects structures near the heel. Because these causes can overlap and build gradually, identifying the specific factors involved is key to choosing the right approach for pain relief.
How do I know if I have heel pain?
Heel pain often starts as an aching or sharp sensation at the back or bottom of the heel, particularly when you take your first steps in the morning or after a prolonged period of rest. While the pain might abate as you move around, it can return after walking, running, or standing for long periods. You might also notice swelling, tenderness, or stiffness in the heel, especially after rest. In some cases, pain becomes more noticeable when wearing shoes that don’t offer enough support or cushioning. If the pain persists or begins to affect how you move throughout the day, it’s advisable to consult a podiatrist for a closer look at what might be the cause.
Do shoes matter when it comes to heel pain?
Yes, the type of footwear you put on can influence how much pressure your heels are exposed to throughout the day. Supportive shoes help cushion each step and reduce strain on the structures around the heel, especially during walking or standing for long periods. That said, the right shoe depends on factors like foot shape, activity level, and how you walk. If heel pain has been a recurring issue, it’s worth reviewing your footwear with a podiatrist who can recommend styles with the structure, cushioning, and support best suited to your needs.
What can a podiatrist do to help with heel pain?
At Straits Podiatry, we offer a range of services to support individuals experiencing heel pain. Each approach is guided by a detailed assessment and tailored to the person’s specific needs. The goal is to reduce strain, improve foot function, and support long-term comfort. Some of the things we offer include:
- Custom Foot Orthotics: These shoe insoles are designed to provide support for the heel and arch. They help redistribute pressure foot to reduce movement discomfort.
- ESWT: This non-invasive technology uses focused acoustic waves to stimulate healing in tissues that might be under long-term strain and pain.
- EMTT: This non-invasive technology uses electromagnetic pulses to support tissue repair and reduce inflammation in areas affected by repetitive stress.
- Exercise Guidance: Where appropriate, podiatrists will advise on stretching or strengthening exercises that support flexibility, stability, and overall foot mechanics.




