Straits Podiatry
Leg & Foot Pain Clinic For Children And Adults
Ahli Perubatan Healthway
Straits Podiatry
Leg & Foot Pain Clinic For Children And Adults
Ahli Perubatan Healthway
Recover With Podiatry
Straits Podiatry is the leading podiatry practice in Singapore, providing dedicated care for patients of all ages. From paediatric concerns like flat feet and walking difficulties to adult issues such as lower limb musculoskeletal and soft tissue conditions, diabetic foot problems, and age-related mobility changes, our team offers personalised care across a wide range of podiatric conditions. With clear communication and evidence-based approaches at the core of what we do, our team of skilled podiatrists work to relieve pain, restore comfort, and help you stay active.
Your Foot Care Starts Here
TIADA STEROID, TIADA PEMBEDAHAN, TIADA DOWNTIME
Our Philosophy in Foot Care


“Three words to describe Straits Podiatry - ACE: Attentive, Caring, and Efficient!"
Amita Berthier, Pelapis Olimpik Singapura


BERPENGALAMAN PAKAR ANGGOTA BAWAH, KAKI DAN BUKU LALI DI SINGAPURA
Podiatrists Kami
Dr Saw Yu Ting
Encik Jackie Tey
BERPENGALAMAN PAKAR ANGGOTA BAWAH, KAKI DAN BUKU LALI DI SINGAPURA
Podiatrists Kami
Saw Yu Ting
Ms Saw Yu Ting
Jackie Tey
Encik Jackie Tey
Benedict Khoo
Encik Benedict Khoo
Maggie Lee
Ms. Maggie Lee
Mr. Daniel Wong
Mr. Daniel Wong
Proses 4 Langkah Kami Pada Lawatan Pertama Anda
Kami menjaga pesakit kami setiap langkah. Inilah yang diharapkan pada lawatan pertama anda.

Podiatrist anda akan mendengar kebimbangan anda dan bertanya kepada anda soalan yang diperlukan yang berkaitan dengan keadaan ini

Podiatrist anda akan melakukan ujian yang diperlukan untuk memeriksa lebih lanjut. Ini mungkin melibatkan penggunaan pengimejan ultrasound diagnostik.

Podiatrist anda akan menerangkan diagnosis dan mengesyorkan pelan rawatan terbaik yang disesuaikan dengan keadaan anda.

Kami menyediakan diagnosis dan rawatan pada hari yang sama. Setelah menerima persetujuan anda, Podiatrist kami akan memulakan rawatan anda.
Artikel yang anda mungkin suka
As podiatrists, one of the pieces of advice that we constantly give is to choose the right footwear. Good shoes are essential for maintaining good foot health and overall comfort. It provides the support and protection your feet need, whether you are walking, running, or standing for long periods. Wearing the right shoes can also prevent injuries, especially during exercise, reduce foot pain, and improve your quality of life. In this blog, we’ll provide expert advice on choosing the right footwear and discuss the key features that make a good shoe for your feet.
Overview of Footwear
Footwear should be seen as more than just a fashion statement or a way to protect the skin of your feet. Your footwear influences your gait pattern, overall health, and well-being. Poorly designed or ill-fitting shoes can contribute to a wide range of foot problems, such as plantar fasciitis, bunions, metatarsalgia, or ankle sprains.
On the other hand, a good pair of shoes provides the proper support, cushioning, comfort, and alignment to control and stabilise our foot joints.
When selecting footwear, it’s important to keep in mind the activity you’ll be performing, your specific foot shape, and any existing foot issues. If you need a more personalised recommendation, podiatrists can help. They can assess your foot posture and foot health, and recommend the best choice for your feet.
What Makes a Shoe?
Heel Counter
The heel counter is the stiff, supportive material at the back of the shoe that surrounds and holds the heel in place. It prevents your heel from moving excessively when walking, providing stability that is very important for people with flat feet. A good heel counter helps prevent injuries like ankle sprains and provides overall foot stability, especially during high-impact activities.
Shoe Upper
The shoe upper refers to the portion of the footwear that covers the top of the foot. It is made from various materials such as leather, mesh, or synthetic fabric, and its primary function is to hold the footwear securely on the foot. A good shoe upper should be breathable and flexible to allow for comfort and ventilation while still providing enough support and structure to keep the foot in place.
Insole
The insole sits in the shoe directly under the foot, also known as the footbed. Insoles provide cushioning and support, enhancing comfort by absorbing shock with every step. They can be made from a variety of materials, such as foam, gel, or cork. Many shoes nowadays come with removable insoles, allowing you to replace them with custom orthotics for additional support or to address specific foot conditions.

Midsole
The midsole is the layer between the insole and the outsole of the shoe, often made of EVA (ethylene-vinyl acetate) foam, silicone gel, or other soft cushioning materials. Its main role is to provide shock absorption and stability, helping to protect the feet, knees, and joints from ground impact. Many sports shoes now feature a highly engineered midsole, including features like arch support and enhancements that alter pressure distribution to improve comfort and performance, especially during running or high-impact activities.
Shank
The shank of the shoe is like a stiffener at the centre of the midsole. The purpose of a shank is to control the amount of torsion and flexibility of the footwear. Our midfoot is not meant to move much and should be firm and stable as we propel forward. A stiff shank will provide a stable platform for the foot to rest on.
Outsole
The outsole is the bottom-most layer of the shoe that comes into direct contact with the ground. Typically made of durable rubber or a rubber composite, it provides traction, stability, and durability. A well-designed outsole helps prevent slipping and enhances grip on various surfaces, making it especially important for outdoor or sports-related footwear. The outsole design can differ when the intended terrain of use is different. For example, a hiking shoe’s outsole is usually made of higher-density rubber with deep grooves to enhance traction.
Toe Box
The toe box is the front part of the footwear that houses the toes. A good toe box should offer enough room to allow for natural toe movement, providing a comfortable fit and preventing issues like bunions or hammer toes. A narrow or cramped toe box can lead to discomfort or even deformities over time.
Fastener
The fastener helps to secure the foot in the shoe and allows one to adjust for a snug fit. Various fastening systems are available in the current market, ranging from shoelaces to velcros and elastic bands. A good fastener provides a secure, snug fit while still allowing room to accommodate different foot shapes. It can also enhance comfort and prevent foot slippage, reducing the risk of blisters and instability.

Types of Footwear
Footwear is designed for specific purposes, and each type offers unique features that support the intended activities. Wearing a shoe that is not meant for the intended activity can cause harm; hence, you should avoid doing so. Here are some common types of footwear:
- Casual Shoes: These are footwear that should be worn just for everyday walking, such as commuting to work or shopping. Sneakers and slip-ons are some casual shoes you can easily find. They should provide basic support and cushioning to ensure comfort for extended wear.
- Athletic Shoes: These sports shoes or trainers are engineered to provide superior support, stability, and cushioning. These footwear also incorporate designs that offer different levels of traction and stability for specific sports, such as basketball or tennis.
- Work Shoes: These footwear are purely used for work, such as safety boots. If you must stand or walk for long periods at work, your shoes must offer sufficient arch and midfoot support and cushioning. Some work shoes may include features like slip resistance, steel-cap toe protection, or “orthopaedic” support.
- Dress Shoes: While these are often more for formal wear, dress shoes should still provide adequate support, especially if worn for long durations. We recommend choosing dress shoes with a low heel, a rubber heel post (instead of wood), soft upper material, and a rounded toe box.
- Orthopaedic Shoes: Frankly, “orthopaedic” footwear does not exist. They are often called “orthopaedic” shoes because they have features that can help individuals with orthopaedic foot conditions like bunions, flat feet, or arthritis. These footwear generally offer more arch support, cushioning, and stability to help relieve foot pain and make walking more comfortable.
Features of a Good Shoe
A good shoe should, at the minimum, fit your feet well. It should also support your foot structure and function. Here are some key features to look for when choosing the right footwear:
- Arch Support: Proper arch support helps relieve foot stress and prevents excessive pressure on the plantar fascia. A shoe with good arch support can alleviate pain and avoid long-term foot issues.
- Cushioning: Shoes with ample cushioning help absorb shock, reducing impact on the joints and soft tissues, especially during running or high-impact movements. Look for shoes with cushioned insoles or midsoles to improve comfort.
- Proper Fit: A good shoe should fit snugly without being too tight. There should be enough room and width in the toe box to prevent forefoot compression. A poorly fitted shoe can cause blisters, bunions, Morton’s neuroma, or other foot deformities.
- Firm Heel Counter: A stable heel cup and supportive heel height help control the heel movements and prevent excessive strain on the foot’s ligaments and tendons.
- Flexibility and Stability: A good shoe should be flexible in the forefoot area (where the toes bend) while providing enough stability in the midfoot and heel. Shoes that are too stiff or overly flexible can lead to imbalances and discomfort.
- Breathability: Shoes upper that are made of breathable materials, such as mesh or leather, help to reduce moisture buildup. This can reduce foot odour, and prevent fungal nails and skin infections or blisters.

Importance of Wearing the Right Shoe
Wearing the right shoe can be considered a form of treatment. Sometimes, changing a pair of shoes is all you need to relieve your foot pain. Proper footwear is also crucial for several reasons:
- Prevention of Foot Problems: A good shoe will support and fit the feet well, improve gait functions, and reduce the risk of developing foot pain or deformities.
- Enhanced Comfort: The right shoe can provide the necessary cushioning and support to ensure your feet remain comfortable throughout the day.
- Improved Posture and Balance: Proper footwear helps control joint movements, cushion impact and prevent discomfort in the knees, hips, and lower back. A stable shoe also improves overall balance and prevents slipping.
- Injury Prevention: Wearing a good shoe that fits properly and provides the right level of support can help prevent injuries, such as sprains, strains, and stress fractures, particularly during physical activity.
How Can Shoes Prevent Injury?
Wearing the correct footwear can significantly reduce the risk of injuries, particularly those related to overuse or trauma. Here are a few ways that good shoes help prevent injury:
- Shock Absorption: Properly cushioned shoes help absorb the impact of running and jumping, preventing excessive strain on the joints, ligaments, and muscles.
- Support and Alignment: Shoes with proper arch support and heel stability help maintain natural foot alignment, reducing the risk of shin splints, knee pain, and lower back discomfort.
- Supports Specific Movements: Shoes that are designed for specific sports come with features that protect your feet while taking part in the sport. For example, basketball shoes tend to be higher cut to prevent ankle sprains.
Kesimpulan
Wearing the right footwear is the best way to maintain foot health and prevent injury, comfort, and mobility. A good shoe should provide the support, cushioning, and stability your foot needs. It also takes stress off the foot and makes being on feet more comfortable. Whether you’re engaging in physical activity, working long hours, or simply walking around, the right shoe can make a significant difference.
When choosing shoes, it’s really important to consider your foot type, the activity you’ll be doing, and any existing foot issues you may have.
If you have specific foot concerns or need personalised recommendations, consult a podiatrist at Straits Podiatry to make the best choice for your feet. Take care of your feet by investing in good shoes that provide the comfort you need for a healthier lifestyle. Contact us today!
Plantar fasciitis is arguably the most common cause of heel pain and foot discomfort. It typically results from inflammation of the plantar fascia, which is a band of tissue responsible for supporting the foot arch. Although plantar fasciitis can be painful and disrupt daily activities, it can be “cured” in terms of being pain-free. With the right approach, most individuals can recover and return to activities. In this article, we’ll dive into the overview of plantar fasciitis and its symptoms and recommend some home remedies you can try.
Overview of Plantar Fasciitis
Plantar fasciitis arises when the plantar fascia is inflamed and degenerated due to excessive strain. The plantar fascia helps absorb shock and support the arch of your foot as you walk, run, or stand. Small tears can occur when this tissue is overused or under too much pressure, leading to inflammation and pain, typically at the heel.
The condition usually results from repetitive strain or overuse, especially in people who engage in high-impact activities like running or jumping. However, it can also develop due to poor footwear, obesity, flat feet, or other biomechanical issues that stress the foot more.
Tanda dan Gejala
The hallmark symptom of plantar fasciitis is stabbing pain under the heel, primarily when taking the first steps in the morning or after a period of rest. This pain usually decreases as the foot warms up but may return after prolonged standing or physical activity. Other common symptoms include:
- Swelling or tenderness around the heel or arch area.
- Stiffness and discomfort when walking after long periods of inactivity.
- Pain after exercise, especially if the activity involves running, walking, or standing on hard surfaces.
Does Plantar Fasciitis Go Away on Its Own?
In some cases, plantar fasciitis may improve on its own with rest and self-care measures. This commonly occurs when it is the first time you are experiencing the symptoms, and can usually last a few weeks.
However, for many people, the pain can persist for months or even years without medical management. It’s important to address the issue early to prevent the condition from becoming too chronic.
While some individuals may notice a decrease in pain after a few weeks of self-care, others may require professional treatment. Ignoring the pain and continuing high-impact activities without addressing the inflammation can lead to more severe symptoms and a longer recovery period. Unfortunately, it is far too often that people try to “walk” the pain off, making management more tricky.

What Should I Do if My Pain Is Not Improving?
If your plantar fasciitis pain is not improving with rest and basic self-care, it may be time to seek plantar fasciitis treatment. Here are some home remedy options you can try:
- Stretching and Exercises: Exercises for plantar fasciitis aim to improve the flexibility of calf muscles, reduce the tension of the plantar fascia, and increase the load endurance of the plantar fascia.
- Night Splints: Wearing night splints helps stretch the plantar fascia while you sleep and is a proven method to help relieve pain on first step.
- Choosing the Right Shoes: Wearing shoes with high cushioning properties helps to reduce shock on the heel. It is also essential to avoid walking barefoot as much as possible.
Can I Get Plantar Fasciitis Again?
Yes, you can experience plantar fasciitis again, especially if the underlying causes are not addressed. Common factors that increase the likelihood of recurring plantar fasciitis include:
- Improper Footwear: Wearing shoes that lack support or don’t fit properly can contribute to the development of plantar fasciitis.
- Overuse: Doing too much high-impact activities without sufficient rest place excessive stress on your feet, especially running or standing for long periods, which can increase the risk of recurrence.
- Obesity: High body weight places additional stress on the feet, making it more likely for the plantar fascia to become inflamed again.
- Biomechanical Issues: Flat feet, high arches, or abnormal walking patterns can place additional strain on the plantar fascia, increasing the risk of recurrence.
To prevent re-injury, you need to address and target all the factors that are causing the condition. That may include the shoes you wear, the exercises you should do, and maintaining a healthy weight. If you have any underlying foot posture or biomechanics issues, a pair of custom orthotics may also be necessary.
Kesimpulan
Plantar fasciitis is a common cause of heel pain that can significantly impact one’s ability to walk, run, and perform daily activities. While the condition may resolve on its own for some, others may require treatment to alleviate pain and promote healing. With early intervention, most people can recover completely and return to normal activities. However, ignoring the condition or failing to address its underlying causes can lead to chronic pain and more serious complications.
If you are experiencing persistent heel pain, don’t wait for it to go away on its own. Contact us at Straits Podiatry for a comprehensive evaluation today. Let us get you back on your feet without pain.
Turf toe is a common injury that results in pain and swelling in the big toe, often caused by trauma or excessive force on the joint. While the name might sound unique, this injury is particularly prevalent in athletes who engage in sports that require quick stops, starts, or heavy pushing off, such as football, soccer, and basketball.
Understanding the causes, symptoms, and treatment options for turf toe is essential to properly manage the condition and prevent further damage. In this article, we will discuss the various aspects of turf toe, including its causes, symptoms, treatment, and how to prevent this injury from affecting your athletic performance.
What is a Turf Toe?
Turf toe refers to a sprain or injury of the metatarsophalangeal joint (MTPJ), the joint at the base of the big toe. It occurs when this joint is hyperextended—meaning it is forced to bend upwards beyond its normal range of motion—causing damage to the soft tissues, ligaments, or tendons around the joint. The injury typically results from an impact or trauma to the toe. It is most common in athletes who play on hard artificial turf (hence the name “turf toe”).
While the injury mainly affects the big toe, turf toe can cause significant pain and limit mobility, especially during activities that require running or pivoting.
Causes of Turf Toe
The primary cause of turf toe is a sudden or forceful impact that pushes the big toe backwards beyond its natural range of motion. Common causes include:
- Direct Trauma: The toe may be jammed, stepped on, or bent backwards during a sports-related incident, such as the foot catching on artificial turf or a tackle. It can also be an accidental trauma, such as stubbing the big toe against the door.
- Repetitive Stress: Continuous pushing off, especially when running or sprinting, can lead to strain on the big toe joint. Over time, this repetitive motion can cause damage to the ligaments, resulting in turf toe.
- Overextension: Engaging in sudden movements, such as pushing off too forcefully or rapidly changing direction, can lead to hyperextension of the big toe, which leads to inflammation and injury.

Faktor Risiko
Several factors can increase the likelihood of experiencing turf toe:
- Playing on Artificial Turf: Artificial surfaces, such as synthetic turf, increase the risk of turf toe because they offer less cushioning than natural grass. When players push off from these surfaces, it increases the risk of hyperextending the toe.
- Footwear: Wearing improper or inadequate shoes that lack support or flexibility can increase the risk of turf toe. Shoes with insufficient cushioning or stiff soles make it more difficult to absorb shock, leading to excessive stress on the big toe.
- Sports Participation: Turf toe most commonly affects athletes who participate in high-impact, contact sports such as football, soccer, and basketball, as these activities involve sudden stops, starts, and quick directional changes.
- Previous Injuries: Individuals who have previously experienced toe injuries, particularly those involving the MTP joint, are at a higher risk of developing turf toe due to weakened ligaments or tendons.
Tanda dan Gejala
The symptoms of turf toe typically develop immediately after the injury but may worsen with continued physical activity. Common signs and symptoms include:
- Pain and Tenderness: The injured area, especially around the base of the big toe, may become painful, tender to the touch, and aggravated by movement.
- Swelling and Bruising: The toe may appear swollen or bruised, particularly around the joint.
- Stiffness: Reduced flexibility in the toe joint can make it difficult to move or bend the toe normally.
- Difficulty Walking: Because the big toe is crucial for walking, running, and pushing off during sports, a turf toe can make it difficult to perform these motions without discomfort or instability.
Treatment Options for Turf Toe
The treatment for turf toe focuses on reducing pain, promoting healing, and preventing further damage. Common treatment options include:
- Rest: Resting the injured foot and avoiding activities that put pressure on the toe, such as running or jumping, is crucial for allowing the joint to heal.
- Ice: Applying ice to the injured area can help reduce swelling and alleviate pain. Ice should be applied for 15-20 minutes several times a day during the initial 48-72 hours following the injury.
- Compression and Elevation: Apply compression with a bandage and elevating the foot can help reduce swelling and prevent further injury.
- Anti-Inflammatory Medications: Over-the-counter painkillers can help manage pain and inflammation in the short term.
- Buddy Taping: In some cases, taping the injured toe to the adjacent toe can provide support and stability while the injury heals.
- Physical Therapy: Once the initial pain subsides, physical therapy may be necessary to help strengthen the muscles and ligaments around the joint, restore flexibility, and prevent future injuries.
- Custom Orthotics: In cases of persistent discomfort, custom insoles can help reduce stress on the big toe joint during activities.
- Immobilisation: In more severe cases, a rigid shoe, boot, or brace may be necessary to immobilise the joint and prevent further hyperextension during the healing process.
- Surgery: Surgery is rarely required unless the ligaments are torn or the injury causes long-term instability in the joint.

Can Turf Toe Happen in Other Toes?
While turf toe most commonly affects the big toe, it can also happen in the other toes, although this is less common. The term “turf toe” specifically refers to the injury at the base of the big toe, but similar trauma or hyperextension can occur in the other toes, especially when subjected to excessive force during physical activities. Injuries to the other toes would typically involve the joints or ligaments in those areas, and treatment would follow similar principles, focusing on rest, ice, and immobilisation.
When to See a Podiatrist?
If you are experiencing big toe pain that is severe, persistent, or accompanied by swelling and bruising, a podiatrist can help. A podiatrist can assess and manage your big toe pain and recommend seeking imaging tests, such as X-rays, to rule out fractures or other injuries. Early intervention can prevent the condition from worsening and help you recover more quickly.
You should see a podiatrist if:
- You had a recent trauma to the big toe and is causing persistent discomfort.
- You experience severe pain or swelling in the big toe following an injury.
- You have difficulty moving your toe or walking without discomfort.
- Your symptoms persist despite rest and home care.
- You suspect a more severe injury that might involve ligament or tendon damage.
Kesimpulan
Turf toe is a painful injury that can limit your ability to take part in sports and daily activities. Understanding the causes, symptoms, and treatment options is crucial for managing the condition and recovering quickly. Our recommendation is to seek timely medical attention and following the management plan, so you can prevent long-term complications and get back on your feet sooner.
If you’re experiencing big toe pain or suspect a turf toe injury, consult our podiatrist at Straits Podiatry for expert care and tailored solutions to help you recover and avoid future injuries.
Offloading diabetic foot ulcers refers to some methods used to relieve pressure from an ulcerated area of the foot. Offloading an ulcer is important because excessive pressure on the foot can worsen ulcers, delay healing, and increase the risk of complications.
Unfortunately, over 80% of lower-limb amputations in diabetic patients are preceded by foot ulcers. One important method of offloading is Total contact casts (TCC). However, studies show that only 1.7% of clinics use TCCs. Moreover, about 45.5% of clinics do not use TCCs to treat diabetic foot ulcers. [1][2][3]
In this article, we will shed some light on some practical strategies for offloading diabetic foot ulcers. By the end of this post, you will learn everything there is to know about this topic.
Types of offloading devices
There are different offloading devices that suit specific types of ulcers and patient needs. The choice of the right device depends on the ulcer’s location, the patient’s mobility, and the presence of infection.
Total Contact Cast (TCC)
Total contact casts are considered the gold standard for offloading diabetic foot ulcers, especially for ulcers present on the plantar (bottom) aspect of the foot.
If you are unfamiliar with this device, it looks like a leg cast for fractures. A TCC is a specialised cast that evenly distributes pressure across the entire foot and lower leg. The goal is to keep the leg suspended and minimise pressure on the ulcerated area. According to a 2015 randomised clinical trial, the effectiveness of TCCs can heal 72% to 100% of ulcers within 5 to 8 weeks. [4]
Removable Cast Walkers (RCW)
Removable cast walkers are another option for offloading. They are removable, allowing practitioners to inspect the wound and change the dressings regularly.
Patients often prefer these devices because of their convenience. However, their effectiveness mainly depends on your compliance. Additionally, researchers found that inconsistent wear of RCW dramatically reduces the benefits of these devices. [5]
Healing sandals and half shoes
Healing sandals (i.e., post-op shoes) are special footwear that offloads pressure from the forefoot or rear foot by redistributing weight to the non-ulcerated parts of the foot. These shoes do not offload pressure as effectively as the above methods, but they are simple and easy to use. However, the effectiveness is also highly dependent on patient compliance.
Crutches and wheelchairs
For patients with severe ulcers, crutches or wheelchairs can also be an effective offloading method. These devices eliminate pressure on the foot and remove the need for the patient to walk on the ulcerated area.
How to properly effectuate offloading
Offloading is not just about the application of a device. It also involves a comprehensive approach that requires considerations such as the patient’s health, lifestyle, and specific needs.
Here are some practical steps to ensure effective offloading:
Choose the right device
The choice of the offloading device is ultimately the most important factor that affects effectiveness. However, it is almost impossible to always offer the gold standard option to every patient. We need to consider factors such as the ulcer’s location, the patient’s mobility, and the presence of any other health issues. For instance, TCCs are ideal for plantar ulcers but may not be suitable for patients with poor balance or severe infections.
Follow the right instructions
The effectiveness of offloading devices depends on their correct application. Researchers show that offloading devices may potentially create new pressure points, which can trigger new ulcers. Therefore, it’s indispensable for healthcare providers to be trained in using these devices. Only then, it will be possible for them to teach patients. [6]
Monitor and adjust regularly
The offloading device needs to be monitored. These devices may exacerbate diabetic foot ulcers when they are not used properly. An examination should focus on frequent checks for signs of new ulcers, adjustments to the device as needed, and regular dressing changes.
Educate the Patient
A multidisciplinary team will ensure the patient is properly educated about their condition. Patients must understand why they need to use the offloading device consistently. At the same time, behaviours that could compromise their treatment (e.g., walking with the device, not following wound care instructions) must be avoided.
Address compliance issues
One of the biggest challenges with offloading is patient compliance. Removable devices like RCWs are less effective if patients do not wear them consistently. Therefore, it is vital to emphasise the importance of wearing the device clearly and consistently during regular follow-up appointments.
Why multidisciplinary care for diabetic foot ulcers is important?
The successful management of diabetic foot ulcers requires a multidisciplinary approach. This involves the collaboration between various healthcare providers, including podiatrists, orthopaedic surgeons, vascular surgeons, endocrinologists, and nurses. Each professional plays a role in ensuring the ulcer is treated effectively.
The central points of multidisciplinary care:
- Frequent foot examinations by healthcare providers.
- Infection control involves rapid treatment of any infections.
- Proper wound care and dressing applications.
- Patient education about foot care and the importance of offloading
Mesej bawa pulang
Offloading is a cornerstone of diabetic foot ulcer treatment. This method reduces the pressure on the ulcer and accelerates wound healing. We understand that the different offloading methods may be overwhelming for you. However, the key to success is wearing the device correctly and following instructions.
Hopefully, this article helps you understand the importance of offloading diabetic foot ulcers and how to practice it.
If you are or know someone facing difficulty dealing with diabetic foot ulcers, feel free to contact us. Our multidisciplinary team at Nobel Diabetic Foot Care will strive to provide a holistic management plan tailored to your needs.
Rujukan
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10723802/
- https://www.hmpgloballearningnetwork.com/site/wounds/article/clinical-and-economic-benefits-healing-diabetic-foot-ulcers-rigid-total-contact-cast
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2571059/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7950500/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9837274/
- https://www.researchgate.net/publication/366439273_Offloading_Devices_for_the_Prevention_of_Heel_Pressure_Ulcers_A_Realist_Evaluation
A diabetic foot infection is a serious complication of diabetes that can cause devastating consequences.
When you have diabetes, your body’s ability to heal wounds is compromised, especially in your feet. This is mainly due to poor blood circulation and nerve damage. Once an infection sets in, it can quickly escalate, which causes serious complications such as ulcers, bone infections, and amputation.
Let’s take a look at some numbers: [1]
- Roughly 25% of people with diabetes will develop a foot ulcer in their lifetime.
- 60% of all lower limb amputations are related to diabetic foot infections.
- People with diabetes are five times more likely to be hospitalized for a foot infection compared to those without diabetes. [2]
The risk factors of diabetic foot infections
Certain factors increase the risk of diabetic foot infections, which include:
- Poor blood sugar control can damage nerves and blood vessels. Ultimately, this reduces your body’s ability to heal wounds.
- Peripheral neuropathy causes loss of sensation in the feet, which makes it difficult to notice injuries.
- Poor circulation reduces blood flow to the feet, which slows down wound healing.
- Foot deformities (e.g., bunions, hammertoes) create pressure points on the feet. This can cause sores that may become infected.
The possible outcomes of diabetic foot infections
Cellulitis
Cellulitis is a bacterial skin infection that develops when the infection spreads from the initial wound into the surrounding skin and tissues. This condition causes redness, swelling, warmth, and pain. The infection can quickly propagate to nearby tissues without appropriate treatment, which could be devastating.
One possible complication of untreated cellulitis is gangrene.
Gangrene
Gangrene describes the death of body tissue due to a lack of blood flow. This complication occurs when the infection is severe enough to impair blood flow to the foot. As the tissue dies, it may turn black, and a foul odour will develop.
Gangrene is a medical emergency that requires surgical intervention to save the rest of the limb from necrosis (i.e., tissue death). In fact, debridement and amputation may be the only possible way to save the patient’s life.
Learn more about the relationship between diabetes and gangrene by clicking on this link (insert a link to the previous article).
Increased mortality risk
The presence of a diabetic foot ulcer nearly doubles the risk of death within three years. [3]
Amputation
Approximately 60% of lower limb amputations in people with diabetes are due to infected foot ulcers. After amputation, the five-year mortality rate is around 60%.
Osteomyelitis
This bone infection occurs in about 15% of diabetic foot ulcers. Furthermore, 15% of those cases proceed to amputation.
How to manage diabetic foot infections?
Early detection of foot problems is vital to prevent infections from becoming severe. We strongly recommend regular foot inspections (daily if possible), especially if you have diabetes. Look for any signs of redness, swelling, or sores. See medical attention immediately if you notice any of these symptoms.
Here are some treatment options:
Wound care
The purpose is to keep the wound clean and moist. Proper wound care also involves offloading the pressure from the affected area, which promotes healing.
Antibiotik
If an infection is present, antibiotics are often necessary. However, if poor blood circulation is present, these medications may take longer to be effective.
Surgery
In severe cases, surgery may be necessary to remove infected tissue or amputate the affected limb to stop the spreading of the infection.
The prevention of diabetic foot infections
Prevention is always better than cure. This is why there are several steps you can take to reduce your risk of diabetic foot infections:
- Maintain good blood sugar control.
- Inspect your feet daily and Look for cuts, blisters, redness, swelling, or any other abnormalities.
- Shoes that fit well and protect your feet from injury are essential. Avoid walking barefoot, even at home.
- Visit your healthcare provider or a podiatrist regularly to monitor your foot health and address any issues early.

The importance of regular foot examination
Regular foot examinations play an essential role in the early detection and prevention of serious diabetic foot complications.
Why do regular foot exams matter?
Foot complications in diabetes can develop gradually and may not be immediately noticeable. Small injuries, calluses, or minor infections can quickly blow up to serious conditions due to poor circulation and nerve damage.
What happens during a foot exam?
During a foot examination, a healthcare professional will thoroughly inspect your feet for any signs of damage. They will also check for corns, calluses, and any areas of increased pressure that could cause sores.
Moreover, the healthcare provider will assess your foot’s circulation and check pulses. They may also use a monofilament test to measure your sensitivity to touch, which helps determine the extent of any nerve damage.
If any abnormalities are found, the healthcare provider may suggest specific treatments, such as:
- Wearing custom orthotics to relieve pressure on certain areas.
- The prescription of antibiotics for infections.
- Lifestyle changes to improve circulation.
In some cases, referral to a specialist (e.g., podiatrist, vascular surgeon, orthopaedic surgeon) may be required to further evaluate and manage your condition.
How frequently should you have a foot exam?
The frequency of foot exams depends on your individual risk factors. For most people with diabetes, an annual foot exam is highly recommended.
However, if you have a history of foot ulcers, neuropathy, or circulation problems, more frequent exams (every three to six months) may be necessary.
Mesej bawa pulang
Diabetic foot infection is a serious health risk that could potentially lead to amputation and even death. However, with proper management of blood sugar levels, regular foot care, and early treatment of any foot problems, these risks can be significantly reduced.
We hope this article will serve as a mini-guideline to help you treat and prevent diabetic foot infections.
If you or someone you know are experiencing issues related to diabetic foot, feel free to contact us or our specialists at Nobel Diabetic Foot Care.
A toe pain may sound like a minor issue, but it can be a significant nuisance that disrupts your daily life. It can even make a simple, enjoyable activity like morning walking in the park impossible. You might also find yourself limping with every step or wearing your shoes so carefully to avoid that pain. At this stage, most of you are definitely wondering what could cause so much pain to your toes. Therefore, in this article, we will list some common causes behind your nagging toe pain and provide simple management and prevention strategies that you can try. Understanding various causes of toe pain will allow you to seek help at the right time and receive appropriate treatment.
Top 5 Common Causes of Toe Pain
Toe pain can arise from many root causes, and their symptoms vary depending on the diagnosis. One of the most common causes is arthritis, which is joint inflammation and stiffness due to degeneration. Toe arthritis often results in discomfort during movement, commonly affecting the big toe joint.
Another common cause is a bunion, an abnormal bony bump that forms at the base of the big toe. Bunions can make wearing covered shoes uncomfortable and lead to chronic pain if left untreated.
Sports injuries or trauma can inflict damage on your toes, too. Fractures or sprains occur more often than you might think, especially among active individuals. The usual trauma we commonly see is a turf toe, the big toe joint sprain, usually from kicking against a hard surface.
Besides the bone and joint, the culprit for your toe pain could be the nails. Ingrown toenails are notorious for causing sharp pain when they grow into the skin instead of straight out. This condition may also result in redness, swelling, and infection around the affected area.
Lastly, conditions like gout bring sudden intense pain due to uric acid buildup in joint spaces. The pain can be so extreme that even a blanket touching the toe could wake you up from sleep. Each cause requires attention for proper management and relief.

Gejala-gejala
Toe pain can manifest in various ways, and recognising the symptoms is crucial for effective treatment. Most conditions will give you a sharp or throbbing pain that makes walking uncomfortable.
Swelling around the toe joint also often accompanies this discomfort. The area may feel warm to the touch, indicating inflammation.
Another common symptom is stiffness, which can make bending or straightening your toes difficult. This could be accompanied by a tingling sensation or numbness—hallmark symptoms of Morton’s neuroma.
If you notice any discoloration—like redness or bruising—it’s a sign that something isn’t right. In some cases, blisters or calluses may also develop due to friction from shoes.
If you find it hard to walk without limping, it is time to pay attention to these signals from your body. Ignoring them or “walking it off” might lead to more significant issues down the line.
Toe Pain Treatment
Treatment for toe pain often starts with rest. Giving your toes a break can help reduce inflammation and discomfort. Consider elevating your feet to ease pressure as well.
Ice is another simple yet effective remedy. Applying an ice pack wrapped in a cloth can minimise swelling and numb the pain. Aim for 15-20 minutes at a time, several times a day.
For more persistent issues, over-the-counter pain relievers may provide short-term relief. However, taking these over a prolonged period is not ideal and is a sign to tell you to seek medical help.
If you have bunions or corns, special pads or orthotic devices can alleviate pressure on painful areas. Wearing comfortable shoes that fit well will also make a significant difference. A trained Podiatrist can guide and help you.
Exercise and stretching can be beneficial, too. Focus on exercises that strengthen foot muscles and improve flexibility. This approach aids recovery while preventing future problems from arising.
If the above methods do not provide sufficient toe pain relief, consider seeking proper treatment. Shockwave therapy is an effective option to manage the pain and stimulate natural recovery. Wearing a pair of prescription customised insoles will also be beneficial if the root cause of your pain is your foot posture and gait pattern.

Pencegahan
Preventing toe pains starts with choosing the right footwear for your feet. Choose shoes that provide adequate support and a comfortable fit. Avoid high heels or overly tight styles that can compress your toes.
Regular foot stretching exercises can enhance flexibility and strength. Exercises such as toe curls or ball rolling can help maintain healthy foot function.
Maintaining a healthy weight can help prevent excessive pressure on your feet, reducing the risk of developing foot injuries.
Exercise caution when performing activities that strain your toes. Always wear the right footwear designed for the activity that you are participating.
Lastly, listen to your body. If you feel discomfort during certain activities, take breaks and adjust as needed to avoid further issues down the line.
When to Seek Medical Attention?
If you have been suffering from toe pain for weeks, you should seek help. Pay close attention to your toes and monitor for any swelling, redness, or warmth around the affected area. These could indicate an infection or other severe conditions.
Seek medical attention immediately if you notice any unusual symptoms, such as severe pain that doesn’t improve with rest, difficulty walking or bearing weight on your foot, or visible deformities in your toes. A Podiatrist can assess, diagnose, and provide a management plan tailored to your needs.
Being proactive about managing your toe pain will not only alleviate your current discomfort, but will also help prevent potential further complications. Don’t hesitate to consult our Podiatrist today for peace of mind and effective care when needed.
The plantar fascia is a crucial part of the foot structure that plays a significant role in maintaining stability and supporting movement. When the plantar fascia becomes injured or inflamed, it can lead to substantial pain and discomfort, commonly known as plantar fasciitis. Understanding the functions of the plantar fascia, the causes of inflammation, and how to prevent injury can help you better manage this condition and improve foot health.
At Straits Podiatry, we are dedicated to helping patients with plantar fascia-related issues by offering comprehensive care and treatment options.
What is Plantar Fascia?
The plantar fascia is a thick, fibrous band of tissue that runs along the bottom of your foot, holding your heel bone to the toes together. It acts as a pillar for the foot, cushioning the impact of walking, running, and jumping. The plantar fascia helps support the arch of the foot, keeping the foot stable during gait, making it an essential component of foot functions. When the plantar fascia gets inflamed, it can result in significant heel pain, especially with the first steps taken in the morning.
Functions of Plantar Fascia
The plantar fascia performs several important functions for the foot:
- Arch Support: The plantar fascia helps maintain the foot arch by stabilising it when you walk or stand. This support is crucial for preventing excessive foot flattening or over-pronation
- Shock Absorption: As you walk, run, or jump, the plantar fascia absorbs much of the impact and pressure placed on the foot. It helps distribute the force more evenly across the foot to reduce strain on other structures.
- Facilitates Movement: The plantar fascia plays a significant role during push-off. It helps the foot return to its natural shape after each step, enabling efficient movement and stable propulsion.
- Reduces Muscle Stress: The plantar fascia connects the heel to the toes, providing stability and ensuring the smooth movement of the foot. Its role is to help reduce the load and stress acting on muscles within the foot.

Causes of Plantar Fascia Inflammation
Plantar fascia inflammation typically results from repetitive strain or overuse. Here are some common causes:
- Overuse: High-impact activities such as running, jumping, or prolonged standing can cause irritation and inflammation of the plantar fascia.
- Improper Footwear: Wearing shoes with poor arch support or insufficient cushioning can increase stress on the plantar fascia, contributing to inflammation and discomfort.
- Obesity: Excess bodyweight can increase the load on the feet, which can strain the plantar fascia and lead to inflammation over time.
- Foot Structure Abnormalities: Certain foot deformities, such as flat feet or high arches, can affect the way your bodyweight is distributed across the foot, increasing stress on the plantar fascia and leading to inflammation.
- Tight Muscles: Tightness in the calves, Achilles tendon, or other foot muscles can put additional strain on the plantar fascia, increasing the risk of injury.
- Sudden Increase in Activity: Rapidly increasing physical activity without proper conditioning can overwhelm the plantar fascia, resulting in inflammation.
Perlukan Bantuan? Jumpa Pakar Podiat Kami Hari Ini
Can I Walk Without a Plantar Fascia?
Although the plantar fascia is essential for foot function, there are rare instances where it may be absent due to a history of surgical intervention. Without the plantar fascia, several issues may arise:
- Decreased Shock Absorption: Without the plantar fascia to absorb impact, the joints, bones, and muscles of the foot will have to take extra stress, leading to pain and discomfort.
- Instability: The absence of the plantar fascia may cause instability in the foot, especially during movement. This can result in gait abnormalities and even changes in the shape of the foot.
- Altered Foot Mechanics: The absence of the plantar fascia can change the way you walk, potentially causing problems in the ankle, knee, or hip due to improper alignment.
However, in cases where the plantar fascia is absent, other parts of the foot will usually compensate for its function. Custom orthotics, foot rehabilitation, and carefully managed activity can help relief discomfort and improve foot function.
How to Prevent Plantar Fascia Injury?
Preventing plantar fascia injury and inflammation is key to maintaining healthy feet. Here are some tips to help protect the plantar fascia:
- Wear Proper Footwear: Choose shoes that provide proper arch support and cushioning. Avoid high heels or shoes that lack support, as they can increase strain on the plantar fascia.
- Stretching and Strengthening: Regularly stretch your calves, Achilles tendon, and the bottom of your feet to improve flexibility and prevent tightness. Strengthening exercises for the feet and lower legs can also help protect the plantar fascia.
- Gradual Increase in Activity: If you’re increasing your physical activity, do so gradually. Sudden increases in intensity or duration can overload the plantar fascia and lead to inflammation.
- Maintain a Healthy Weight: Excess weight can put added pressure on your feet, increasing the risk of plantar fascia injury. Maintaining a healthy weight helps reduce strain on the foot’s structures.
- Foot Rest and Recovery: Give your feet adequate rest if you’re engaging in high-impact activities. Taking breaks and incorporating low-impact exercises like swimming or cycling can give the plantar fascia time to recover.
- Use Orthotics: If you have flat feet or other structural abnormalities, consider using custom orthotics to provide additional arch support and reduce stress on the plantar fascia.
Kesimpulan
The plantar fascia is a vital structure in the foot that plays an essential role in supporting movement, absorbing shock, and maintaining foot stability. However, it is prone to inflammation, especially when between ages of 40 to 60s, or with repetitive strain or overuse. Understanding the functions of the plantar fascia, the causes of inflammation, and preventive measures can help protect your feet from injury. If you’re experiencing symptoms of plantar fascia inflammation, such as heel pain, discomfort, or difficulty walking, contact Straits Podiatry today for a comprehensive evaluation and personalised management plan. Our team is dedicated to helping you maintain healthy feet and an active lifestyle.
Pakar kaki berpengalaman dalam pengurusan kaki diabetes dan pencegahan amputasi.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Neuroma Morton adalah keadaan biasa yang menjejaskan saraf di kaki. Ia menyebabkan kesakitan dan ketidakselesaan, selalunya di bebola kaki atau di antara jari kaki. Walaupun rawatan konservatif boleh berkesan untuk ramai pesakit, sesetengah mungkin memerlukan pembedahan jika pilihan bukan pembedahan tidak melegakan simptom mereka. Jika anda mempertimbangkan pembedahan neuroma Morton , adalah penting untuk memahami potensi kesan sampingan, risiko dan implikasi jangka panjang. Di Straits Podiatry, kami menyediakan penjagaan menyeluruh untuk neuroma Morton dan membantu membimbing pesakit melalui semua pilihan rawatan sebelum menjalani pembedahan. Inilah semua yang anda perlu tahu tentang pembedahan neuroma Morton.
Apakah Neuroma Morton?
Neuroma Morton ialah pertumbuhan tisu saraf yang jinak (bukan kanser) yang biasanya terbentuk di antara jari kaki, selalunya antara yang ketiga dan keempat. Keadaan ini biasanya disebabkan oleh kerengsaan, mampatan, atau kecederaan pada saraf. Penebalan tisu di sekeliling saraf membawa kepada kesakitan yang tajam, sensasi terbakar, kebas, dan rasa ketulan atau sesuatu di dalam kasut. Ia paling biasa berlaku pada individu yang memakai kasut yang ketat, terlibat dalam aktiviti berimpak tinggi, atau mengalami kecacatan kaki seperti bunion atau gerbang tinggi.
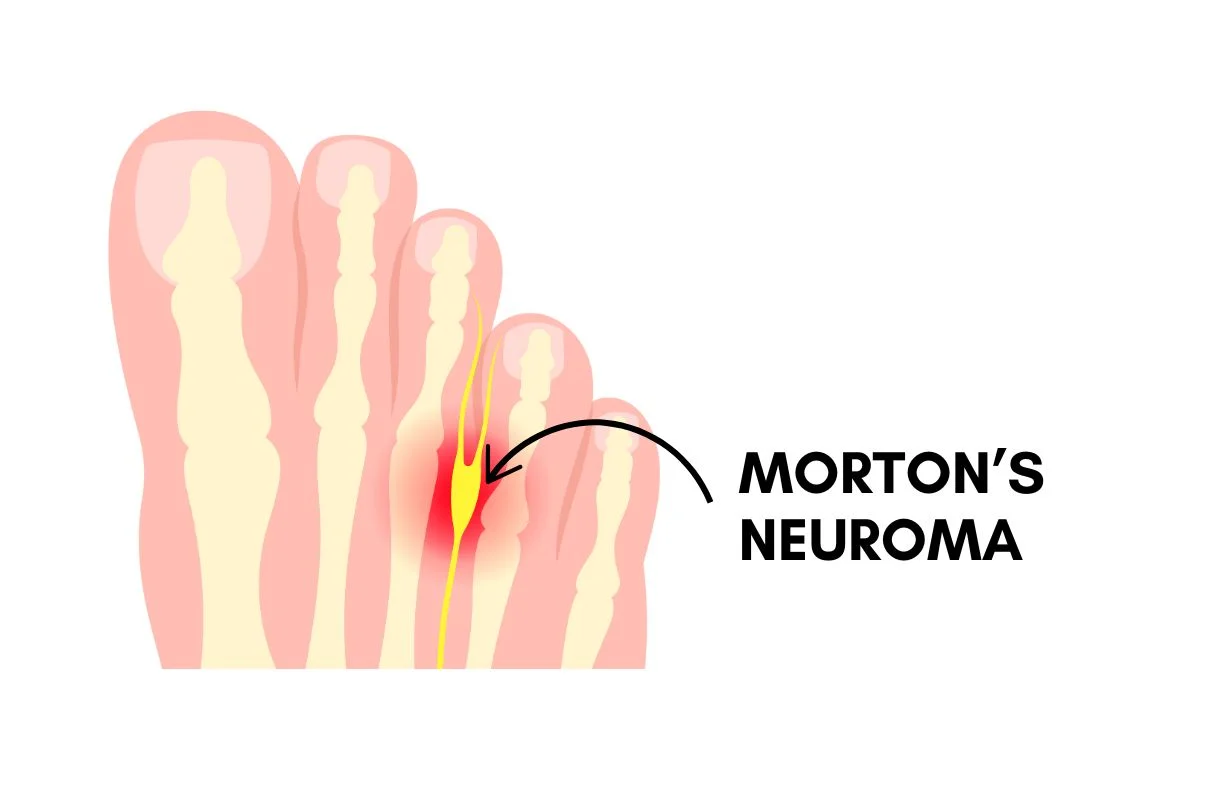
Gejala Neuroma Morton termasuk:
- Sakit yang tajam atau terbakar di bahagian bebola kaki
- Kesemutan atau kebas antara jari kaki
- Sensasi berjalan di atas kerikil atau mempunyai sesuatu di dalam kasut
- Sakit yang bertambah teruk dengan aktiviti atau memakai kasut yang ketat
Bilakah Anda Perlu Pertimbangkan Pembedahan Neuroma Morton?
Pembedahan untuk neuroma Morton biasanya disyorkan hanya apabila rawatan konservatif, seperti berehat, menukar kasut, tapak kaki tersuai , terapi gelombang kejutan atau suntikan, gagal memberikan kelegaan. Keputusan untuk menjalani pembedahan biasanya dibuat selepas beberapa bulan rawatan bukan invasif tidak menunjukkan tanda-tanda peningkatan.
Anda boleh mempertimbangkan pembedahan neuroma Morton jika:
- Kesakitan berterusan selepas meletihkan rawatan bukan pembedahan yang tersedia
- Anda mengalami kesukaran yang ketara dengan aktiviti harian kerana sakit kaki
- Gejala adalah teruk dan melumpuhkan
- Langkah konservatif tidak meningkatkan kualiti hidup anda
Perlukan Bantuan? Jumpa Pakar Podiat Kami Hari Ini
Risiko dan Faedah Pembedahan Neuroma Morton
Faedah:
- Melegakan Sakit : Manfaat utama pembedahan neuroma Morton ialah melegakan kesakitan dan ketidakselesaan yang disebabkan oleh mampatan saraf.
- Kualiti Hidup yang Lebih Baik : Dengan pembedahan yang berjaya, ramai pesakit kembali ke aktiviti harian tanpa rasa sakit yang mengganggu yang sebelum ini mengganggu fungsi kaki mereka.
- Resolusi Jangka Panjang : Pembedahan mungkin memberikan penyelesaian jangka panjang yang lebih baik, terutamanya jika pilihan bukan pembedahan tidak berjaya.
Risiko:
- Jangkitan : Pembedahan sentiasa berisiko mendapat jangkitan di tapak hirisan.
- Kerosakan Saraf : Pembedahan neuroma Morton biasanya melibatkan pengangkatan atau pemotongan tisu saraf yang terjejas, yang boleh merosakkan saraf di sekelilingnya. Ini boleh menyebabkan sensasi yang berubah, kebas, atau kesakitan yang lebih lanjut.
- Berulang : Dalam sesetengah kes, neuroma boleh tumbuh semula, terutamanya jika saraf yang tinggal terus berada di bawah mampatan.
- Pembentukan Tisu Parut : Tisu parut sensitif mungkin terbentuk di sekitar tapak pembedahan, yang membawa kepada ketidakselesaan atau masalah yang berpotensi dengan fungsi kaki.
- Masa Henti : Selepas pembedahan, pesakit mungkin memerlukan masa untuk pulih, dengan sesetengahnya mengalami bengkak, lebam atau sakit semasa proses penyembuhan.
Implikasi Jangka Panjang Pembedahan Neuroma Morton
Walaupun pembedahan neuroma Morton boleh memberikan kelegaan jangka panjang untuk ramai individu, ia bukan tanpa potensi implikasi jangka panjang. Sesetengah pesakit mungkin mengalami:
- Kebas Berterusan : Penyingkiran atau perubahan saraf boleh menyebabkan kebas atau kesemutan jangka panjang pada jari kaki atau bola kaki.
- Perubahan dalam Mekanik Kaki : Mengubah saraf atau tisu sekeliling berpotensi meningkatkan risiko kecederaan selanjutnya pada kaki. Kekurangan sensasi boleh meningkatkan tekanan pada kawasan itu, yang membawa kepada jagung, kapalan, atau sakit sendi.
- Kecacatan Kaki : Walaupun jarang berlaku, pembedahan boleh mengakibatkan perubahan struktur atau penjajaran kaki, yang membawa kepada masalah baharu seperti kaki hammertoe atau claw toe .

Mengapa Pembedahan Harus Menjadi Pilihan Terakhir
Terdapat beberapa sebab mengapa anda harus sentiasa menganggap pembedahan sebagai pilihan terakhir untuk merawat neuroma Morton :
Memperbaiki dengan Rawatan Konservatif
Gejala neuroma Morton biasanya boleh bertambah baik dengan kaedah bukan pembedahan. Terdapat beberapa pilihan yang tersedia, seperti mengubah suai kasut, menggunakan ortotik kaki, terapi gelombang kejutan, atau suntikan. Rawatan bukan pembedahan membawa risiko yang lebih rendah daripada pembedahan dan, oleh itu, harus dipertimbangkan terlebih dahulu.
Risiko Komplikasi
Sebarang kaedah rawatan invasif membawa risiko, termasuk kerosakan saraf, jangkitan, dan pemulihan luka yang berpanjangan. Risiko-risiko ini harus melebihi manfaat bagi pesakit untuk membuat menjalani pembedahan berbaloi.
Pemulihan Selepas Pembedahan
Anda perlu mengambil tempoh rehat selepas pembedahan neuroma Morton, yang boleh mengambil masa antara beberapa minggu hingga beberapa bulan. Anda juga mungkin mengalami kesakitan dan ketidakselesaan pada masa ini. Menetapkan jangkaan anda dengan betul dan menimbang faedah prosedur sebelum menjalaninya adalah kunci.
Kemungkinan Berulang
Walaupun jarang, sesetengah neuroma mungkin kembali walaupun selepas pembedahan. Ini biasanya disebabkan oleh faktor yang tidak dapat diselesaikan yang membawa kepada mampatan saraf yang berterusan. Oleh itu, jika anda sedang mempertimbangkan pembedahan neuroma Morton, anda perlu berjumpa Pakar Podiatri untuk menangani punca keadaan, seperti kecacatan kaki atau kasut yang ketat.
Kesimpulan
Pembedahan neuroma Morton boleh menjadi pilihan rawatan yang berkesan bagi mereka yang tidak mendapat kelegaan daripada rawatan konservatif. Walau bagaimanapun, adalah penting untuk mempertimbangkan potensi risiko, faedah, dan implikasi jangka panjang pembedahan. Di Straits Podiatry, kami mengutamakan pendekatan komprehensif untuk kesihatan kaki dan bekerjasama dengan pesakit kami untuk meneroka semua pilihan rawatan yang ada. Pembedahan hendaklah sentiasa menjadi pilihan terakhir selepas pertimbangan yang teliti dan perbincangan menyeluruh tentang kemungkinan hasil.
Jika anda sedang mengalami simptom neuroma Morton , jadualkan rundingan dengan salah seorang pakar podiatrik kami hari ini. Di Straits Podiatry, pakar podiatri kami akan membincangkan dan membangunkan pelan pengurusan yang disesuaikan dengan keperluan khusus anda. Kami berusaha untuk membantu anda mencapai kelegaan jangka panjang dan meningkatkan kesihatan kaki anda tanpa pembedahan.
Pakar kaki berpengalaman dalam pengurusan kaki diabetes dan pencegahan amputasi.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Orang yang menghidap diabetes mempunyai risiko gangren yang tinggi. Yang terakhir adalah keadaan serius di mana tisu badan mati akibat kekurangan bekalan darah.
Risiko ini meningkat dengan ketara disebabkan oleh kesan diabetes terhadap peredaran darah dan fungsi saraf, yang menjadikannya kritikal bagi individu diabetes untuk berwaspada dalam memantau dan menguruskan kaki diabetes mereka. Malangnya, pesakit dengan neuropati diabetik mungkin tidak menyedari apabila mereka cedera, yang sering membawa kepada jangkitan.
Dalam artikel ini, kita akan membincangkan hubungan antara diabetes dan gangren, termasuk cara mendiagnosis dan mengurus yang terakhir.
Apakah jenis gangren?
Gangrene affects extremities such as toes, fingers, and limbs. However, it may also affect internal organs, muscles or genital areas. It does not only affect diabetic patients, but they tend to be more prone to this condition.
Berikut adalah jenis gangren yang paling biasa yang berlaku pada anggota bawah:
Gangren kering
Gangren kering berlaku apabila aliran darah ke bahagian tertentu badan terganggu kerana peredaran yang lemah. Lesi biasanya kelihatan kering, keriput dan berubah warna (dari coklat ke hitam). Walaupun gangren kering berkembang dengan perlahan, ia menyebabkan komplikasi teruk apabila rawatan yang betul tidak tepat pada masanya.
Gangren basah
Gangren basah dicirikan oleh bengkak, melepuh, dan penampilan basah. Ia biasanya mengikuti jangkitan dan lebih kerap berlaku pada penghidap diabetes kerana tindak balas imun mereka yang terjejas. Dalam erti kata lain, ia adalah tisu yang mati yang dijangkiti. Gangren basah merebak dengan cepat dan boleh membawa maut jika tidak dirawat dengan segera.
Gangren gas
Gas gangrene is rare, and it is caused by a group of bacteria known as Clostridium species. These bacteria produce toxins and gas that precipitate tissue death. The skin over the affected area is usually heavily discoloured (grey, black, and bluish) and swollen with a bubbly texture. It accompanies a strong odour and can be fatal if left untreated.

Faktor risiko dan gejala gangren pada pesakit diabetes
Menurut penyelidikan, diabetes dengan ketara meningkatkan risiko gangren disebabkan oleh komplikasi kaki diabetes berikut: [1]
Penyakit Arteri Periferi (PAD)
Individu yang menghidap diabetes terdedah kepada PAD . Keadaan ini berlaku apabila aterosklerosis menyebabkan pembentukan plak di arteri, yang menyekat aliran darah ke bahagian kaki. Peredaran yang lemah ini adalah faktor kritikal dalam perkembangan gangren.
Neuropati diabetik
Kerosakan saraf yang berpunca daripada paras gula darah yang tinggi boleh menyebabkan kehilangan sensasi pada kaki, yang menjadikannya sukar untuk melihat kecederaan atau jangkitan yang boleh mencetuskan gangren.
Sistem imun terjejas
Tahap glukosa yang tinggi secara kronik melemahkan tindak balas imun.
Gejala gangren berbeza-beza berdasarkan jenis tetapi berikut adalah beberapa yang biasa: [1]
- Perubahan warna kulit (dari merah ke hitam).
- Kesakitan yang teruk diikuti dengan kebas dan terbakar apabila tisu mula mati.
- Bengkak, lepuh, dan pelepasan nanah (kebanyakannya dalam gangren basah).
- A foul-smelling odour that originates from the infected area.
Perlukan Bantuan? Jumpa Pakar Podiat Kami Hari Ini
Bagaimana untuk mendiagnosis dan menguruskan gangren
Early diagnosis is critical to manage gangrene. Medical professionals typically use a combination of physical examinations, blood tests, and imaging studies (e.g., X-rays, CT scans, MRIs) to evaluate the condition. In most cases, surgery will be required to remove the source of the infection and to restore blood flow to the lower limbs.
Pilihan rawatan bergantung pada keparahan dan jenis gangren tetapi secara amnya termasuk:
Debridement
Pembedahan membuang tisu mati untuk mencegah penyebaran jangkitan. Dalam kes yang teruk, ini mungkin melibatkan amputasi anggota yang terjejas. Masa adalah penting apabila menguruskan gangren, campur tangan lebih awal meningkatkan peluang untuk menyelamatkan anggota dan kaki.
Angioplasti
Angioplasti, atau prosedur "belon" selalunya diperlukan untuk membantu memulihkan aliran darah ke kaki yang terjejas dan menghentikan kematian tisu selanjutnya. Ia juga membantu meningkatkan penghantaran antibiotik ke kawasan yang dijangkiti supaya jangkitan dapat dikawal.
Antibiotik
Antibiotik adalah asas gangren kerana ia menghalang penyebaran jangkitan. Malangnya, antibiotik tidak berkesan dalam tisu yang sudah mati (iaitu, mati).
Terapi oksigen hiperbarik
Terapi oksigen hiperbarik ialah modaliti tambahan yang menempatkan pesakit dalam ruang oksigen bertekanan tinggi, yang boleh meningkatkan penghantaran oksigen ke tisu. Prinsipnya adalah untuk meningkatkan ketepuan oksigen dalam tisu dan membolehkan luka pulih.
Jadual di bawah meringkaskan jenis gangren dan rawatan masing-masing:
| Jenis gangren | Ciri-ciri | Rawatan |
| Kering | Kulit kering, kecut dan berubah warna. | Debridement dan kemungkinan amputasi. |
| basah | Kulit bengkak, melepuh, dan keluar nanah. | Debridement, antibiotik, dan terapi hiperbarik. |
| Gas | Kulit berbuih, penyebaran cepat dan gas dalam tisu. | Pembedahan segera dan antibiotik. |
Bagaimana untuk mencegah gangren pada pesakit diabetes?
Pencegahan gangren harus menjadi matlamat setiap pesakit diabetes.
Berikut adalah beberapa langkah praktikal yang boleh anda ikuti:
Pemeriksaan kaki secara berkala – Pesakit diabetes harus memeriksa kaki mereka setiap hari untuk sebarang tanda kecederaan, perubahan warna atau jangkitan. Ini sangat penting bagi mereka yang mempunyai neuropati yang mungkin tidak merasa sakit. Sekurang-kurangnya, berjumpa pakar kaki untuk pemeriksaan kaki diabetes setiap tahun untuk menilai kesihatan kaki anda.
Kawalan gula dalam darah – Pastikan paras gula dalam darah anda berada dalam julat sasaran untuk mengurangkan risiko komplikasi kaki diabetes (cth, PAD, neuropati).
Kasut yang betul – Pakai kasut yang dipasang dengan baik untuk mengelakkan kecederaan kaki yang mungkin tidak disedari dan menyebabkan jangkitan. Amalkan tabiat memakai selipar (menutup jari kaki) di rumah untuk memastikan kaki anda dilindungi.
Berhenti merokok - Merokok memburukkan lagi kerosakan saluran darah, yang meningkatkan risiko PAD dan gangren. Oleh itu, anda mesti berhenti merokok secepat mungkin.
Pemakanan dan senaman yang sihat – Kekalkan berat badan yang sihat, urus paras kolesterol anda dan libatkan diri dalam aktiviti fizikal untuk meningkatkan peredaran darah dan mengurangkan risiko PAD dan gangren anda.
Mesej bawa pulang
Gangren adalah komplikasi serius bagi penghidap diabetes yang boleh menyebabkan amputasi anggota badan. Untuk mengurangkan risiko keadaan ini, pemantauan yang teliti, diagnosis awal, dan rawatan yang sesuai mesti digabungkan. Pesakit diabetes juga mesti proaktif dan berhati-hati terhadap tanda-tanda gangren.
If you suspect yourself or your family members are suffering from symptoms of gangrene, seek help today by contacting us. At Nobel Diabetic Foot Care, we aim to provide timely access and intervention for diabetic foot infections and complications. Our experience multidisciplinary diabetic foot team will provide a holistic tailored treatment plan for you.
Rujukan
- https://www.ncbi.nlm.nih.gov/books/NBK560552/
- https://www.ncbi.nlm.nih.gov/books/NBK549821/
Diabetic foot is a relatively common complication that occurs when blood sugar levels remain elevated for many years or decades. The direct consequences of this condition include numbness, foot ulcers, infections, and foot deformities.
In some instances, the damage can become quite severe. As a result, the infection may spread to nearby tissues and organs. Unfortunately, diabetic foot may lead to amputation if proper intervention is not delivered promptly.
Although most individuals with diabetes do not experience severe foot complications, diabetes continues to be a major cause of amputations.
If you’re not familiar with diabetes, here’s a quick breakdown:
There are two types of diabetes – Type one and type two. Type one diabetes results from an autoimmune reaction where the body attacks the cells in the pancreas that produce insulin. A deficiency in this hormone will cause chronically elevated blood sugar levels. Type two diabetes results from a combination of insulin deficiency and high resistance to its action. [1]
These two diseases are complicated and require a comprehensive approach to treatment. Unfortunately, millions of people do not comply with proper treatment, which causes a high rate of diabetic foot.
In this article, we will go over everything there is to know about diabetic foot, including how it may present and the consequences of not treating this condition.
What you need to know about diabetic foot
Chronically elevated blood sugar levels can progressively harm your nerves, particularly the limbs. Damage to the nerves results in numbness, tingling, and burning sensations. High blood sugar can also speed up the blockage of blood vessels, which causes reduced circulation to your organs. The compromised blood flow can result in heart disease, stroke, kidney issues, and vision impairment.
Damage to nerves impact the sensory feedback in your feet, which causes the following complications:
Neuropati diabetik
According to the Centers for Disease Control and Prevention (CDC), up to 50% of diabetic patients will experience some form of diabetic neuropathy (i.e., nerve damage). When the nerves of the foot get affected, they precipitate something called diabetic peripheral neuropathy. Nerve damage may cause tingling and burning pain in your feet. As the condition progresses, you might lose all sensation in your feet, which makes diabetic neuropathy quite dangerous. [2]
Keep in mind that pain serves as a signal that something is wrong within the body. It can draw attention to cuts, sores, or blisters on your feet. However, with diabetic neuropathy, if you lose sensation in your feet, a cut or blister could go unnoticed for an extended period. Without timely treatment, these injuries can cause serious infections.
Diabetic neuropathy is also the leading cause of diabetic foot ulcers. These ulcers usually develop in high-pressure areas where calluses or corns are present. The lack of sensation does not stop an individual from constantly applying pressure to those areas, leading to tissue breakdown and ulcer formation.
Charcot foot
Charcot foot is a rare condition that arises from uncontrolled diabetes and neuropathy. This usually occurs when an injury (e.g., sprain, fracture) or repeated stress to the foot goes unnoticed due to the lack of sensation caused by peripheral neuropathy. Unfortunately, further walking on the injured foot exacerbates the injury. [3]
Charcot foot is a destructive condition that significantly changes the foot structure. The early symptoms of Charcot foot include swelling, redness, and warmth in the affected foot. As the condition progresses, the bones of the foot start to break, and joints become dislocated and collapse. The foot’s arch also collapses, often resulting in a rounded shape on the bottom of the feet.

Damage to blood vessels also impacts circulation in your feet, which causes the following complications:
Peripheral vascular disease
Diabetes may also contribute to a circulatory disorder called peripheral vascular disease. This cardiovascular condition arises from restricted blood flow to the legs and feet, and blood vessel blockage further limits circulation.
Though this condition can affect anyone, individuals with diabetes face a higher risk because changes in blood vessels commonly disrupt normal blood flow. Additionally, high blood sugar levels can thicken the blood, which makes it harder for it to circulate efficiently.
Gangrene
Peripheral vascular disease also precipitates gangrene, a limb-threatening condition. Diminished blood flow to the feet can stop the healing of sores or infections. Untreated infections may develop into gangrene, which is the death of tissue due to insufficient blood flow.
If gangrene begins to spread to other areas, your doctor may need to amputate a toe, foot, or leg to prevent its progression and infection from spreading.
What are the symptoms of diabetic foot?
Diabetic foot presents with a wide range of signs and symptoms.
Common signs and symptoms include:
- Loss of sensation
- Numbness or tingling
- Blisters or wounds without any pain
- Perubahan warna kulit
- Wounds with or without drainage
- Painful burning sensation
- Redness, swelling, and warmth
If an infection occurs, additional symptoms may occur, including:
- Fever
- A general feeling of being unwell
- Chills
- Uncontrolled blood sugar levels despite treatment
- Shaking
- Shock
- Kemerahan
The table below summarizes the clinical presentation of diabetic foot and its management:
| Presentation | Gejala-gejala | Management plan |
| Loss of sensation | Numbness and tingling, but no pain. | Regular inspections, protective footwear, and patient education. |
| Blisters/wounds | Painless blisters or wounds. | Wound care and topical antibiotics. |
| Skin changes | Skin discolouration. | Circulation evaluation and vascular intervention. |
| Kemerahan dan bengkak | Redness and swelling of the foot and ankle. | Immediate evaluation, possible blood test and x-rays. |
| Wounds with drainage | Open sores and fluid drainage. | Debridement and advanced dressings. |
| Painful tingling | Persistent tingling pain. | Neuropathy medications, pain management, and infection monitoring. |
| Jangkitan | Fever, chills, and redness. | Antibiotics, hospitalization, and surgical intervention if needed. |
| Non-healing ulcers | Persistent ulcers or wounds. | Advanced wound care, offloading, and vascular assessment. |
| Gangrene | Blackened and dead tissue. | Surgical consultation, possible amputation, and infection control. |
| Foot deformity | Structural foot changes. | Custom orthotics, protective footwear, and corrective surgery. |
| Charcot foot | Foot deformity and swelling. | Immobilization, custom footwear, and possible surgery. |
Complications that arise from diabetic foot
Without adequate and prompt treatment, diabetic foot can be extremely severe.
Here are some of the complications that may occur:
- Foot ulcers that do not heal.
- Various types of infections, including skin, bone, and abscesses.
- Gangrene.
- Foot deformities.
- Charcot foot.
- Damage to nearby structures, such as the legs.
In some cases, doctors may be able to reverse complications such as infections. However, more severe complications, such as gangrene, may result in permanent physical changes. Complications often gets more serious with time, therefore early intervention is key to preventing amputations.
Mesej bawa pulang
Diabetic foot is a serious complication that occurs when blood sugar levels are not controlled over a long period. Without proper medical and/or surgical intervention, diabetic foot may precipitate severe complications, including amputation.
We hope that this article has highlighted what you need to know about diabetic foot, including how it presents and what complications it may trigger.
Penjagaan Kaki Diabetes Nobel
If you have diabetes and are concerned about your foot health, we can help you. At Nobel Diabetic Foot Care, we have a team of Orthopaedic surgeons and Podiatrists who provide holistic management of all diabetic foot problems. Our multidisciplinary approach will help minimise any delay in assessment and treatment and ensure that you receive the right care en route to recovery. Don’t hesitate to contact us and schedule an appointment today.
Rujukan
- https://www.cdc.gov/diabetes/about/index.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7096070/
- https://www.ncbi.nlm.nih.gov/books/NBK553110/
Pakar kaki berpengalaman dalam pengurusan kaki diabetes dan pencegahan amputasi.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Sakit tumit boleh menjadi seretan sebenar. Ia boleh menjadikan tugas yang paling mudah, seperti bangun dari katil pada waktu pagi atau berjalan ke kedai, ujian yang menyakitkan. Tetapi jangan risau, anda tidak bersendirian. Ramai orang mengalami sakit tumit pada satu ketika dalam hidup mereka.
Two of the most common causes of heel pain are Achilles Tendonitis and Plantar Fasciitis. While they might sound similar, they’re different conditions with different treatments. In this article, we’ll explore their differences and offer tips for managing heel pain.
Memahami Sakit Tumit
Sakit tumit ialah istilah umum yang digunakan untuk menggambarkan sebarang ketidakselesaan di kawasan tumit. Ia boleh terdiri daripada sakit yang membosankan kepada kesakitan yang tajam dan menusuk. Walaupun tendonitis Achilles dan plantar fasciitis adalah punca biasa, terdapat kemungkinan punca lain, seperti taji tumit atau patah tekanan.
Achilles Tendonitis
Tendonitis Achilles ialah keradangan tendon Achilles, jalur tisu tebal yang menghubungkan otot betis anda ke tulang tumit anda. Ia selalunya disebabkan oleh penggunaan berlebihan, seperti berlari atau melompat.
Gejala tendonitis Achilles termasuk:
- Sakit di bahagian belakang tumit, terutamanya apabila memulakan aktiviti
- Kekakuan pada waktu pagi
- Bengkak di sekeliling tendon Achilles
Plantar Fasciitis
Plantar fasciitis ialah keradangan plantar fascia, jalur tisu tebal yang mengalir di sepanjang bahagian bawah kaki anda, menyambungkan tumit anda ke jari kaki anda. Ia sering disebabkan oleh penggunaan berlebihan atau ketegangan berulang.
Gejala plantar fasciitis termasuk:
- Sakit tajam di tumit, terutamanya pada waktu pagi apabila anda mengambil langkah pertama anda
- Kesakitan yang berkurangan semasa anda bergerak
- Kekakuan di kaki
Perbezaan Antara Tendonitis Achilles dan Plantar Fasciitis
Membezakan antara tendonitis Achilles dan plantar fasciitis boleh menjadi rumit, kerana kesakitan selalunya di kawasan yang sama. Walau bagaimanapun, terdapat beberapa perbezaan utama:
Lokasi kesakitan
Tendonitis Achilles biasanya berada di bahagian belakang tumit, manakala plantar fasciitis biasanya di bahagian bawah.
Apabila Kesakitan Paling Teruk
Kesakitan tendonitis Achilles selalunya lebih teruk selepas aktiviti berat, manakala sakit plantar fasciitis selalunya lebih teruk pada waktu pagi
Bila Perlu Berjumpa Doktor untuk Rawatan Sakit Tumit
Walaupun banyak kes sakit tumit boleh dirawat di rumah, adalah penting untuk berjumpa pakar kaki atau doktor jika:
- Kesakitan anda teruk atau tidak bertambah baik dengan rawatan di rumah
- Anda mengalami bengkak, kemerahan atau kehangatan di sekeliling tumit anda
- Anda mengalami kesukaran berjalan atau meletakkan berat badan pada tumit anda
Pakar kaki atau doktor boleh mendiagnosis punca sebenar sakit tumit anda dan mengesyorkan rawatan yang paling sesuai.
Ambil Langkah Pertama untuk Melegakan Sakit Tumit dengan Podiatri Selat
Sakit tumit boleh memberi kesan ketara kepada kehidupan seharian anda, tetapi ia tidak perlu mengawal anda. Memahami perbezaan antara tendonitis Achilles dan plantar fasciitis adalah penting untuk rawatan sakit tumit yang berkesan. Ingat, walaupun rawatan sampingan boleh memberikan kelegaan sementara, mendapatkan nasihat profesional adalah penting untuk diagnosis yang betul dan pelan rawatan yang disesuaikan.
Straits Podiatry ada di sini untuk membantu anda mengatasi sakit tumit. Pakar kaki kami yang berpengalaman pakar dalam mendiagnosis dan menguruskan pelbagai keadaan tumit, termasuk rawatan tendonitis Achilles dan rawatan plantar fasciitis. Kami menawarkan rawatan sakit tumit yang komprehensif, daripada langkah konservatif kepada terapi lanjutan.
Jangan biarkan sakit tumit menahan anda lagi. Hubungi Straits Podiatry hari ini untuk menjadualkan perundingan.
Are you tired of dealing with those pesky plantar warts? You’re not alone. Many Singaporeans struggle with these stubborn growths on the bottom of their feet. But before you rush to try the latest home remedy or over-the-counter treatment, let’s clear up some common misconceptions about plantar wart removal in Singapore.
Understanding Plantar Warts
Plantar warts are small, rough growths caused by the human papillomavirus (HPV). They often appear on the soles of the feet and can be pretty painful. While they’re not usually dangerous, they can be stubborn and challenging to get rid of.
Common Myths About Plantar Wart Removal
There are many misconceptions surrounding plantar wart removal. Let’s debunk some of the most common myths:
Myth 1: Plantar Warts Are Highly Contagious
It’s a common belief that plantar warts spread like wildfire, but that’s not entirely true. While HPV – the virus that causes warts – can be contagious, it’s not as easy to catch as you might think. Direct contact with an open wart is usually necessary for the virus to spread. So, don’t panic if you see someone with plantar warts.
Myth 2: Plantar Warts Will Go Away on Their Own
Many people hope that plantar warts will magically disappear over time. Unfortunately, this is rarely the case. In fact, if left untreated, plantar warts can become more prominent, more painful, and even spread to other parts of the foot.
Myth 3: Over-the-Counter Treatments Are Effective for Wart Removal
Drugstores are filled with products claiming to remove plantar warts. While some might provide temporary relief, they often fail to completely eradicate the wart. Over-the-counter treatments can also be harsh on the skin, causing irritation and discomfort.
Myth 4: Home Remedies Can Cure Plantar Warts
From duct tape to apple cider vinegar, countless home remedies are touted as plantar wart cures. While some people swear by these methods, little scientific evidence supports their effectiveness. Plus, some home remedies can damage the surrounding skin.
Myth 5: Plantar Warts Are a Sign of Poor Hygiene
Contrary to popular belief, plantar warts are not caused by poor hygiene. Anyone can develop plantar warts, regardless of how often they wash their feet.
Myth 6: Plantar Wart Removal Can Be Done Yourself
Attempting to remove a plantar wart at home can be risky. Improper plantar wart removal can lead to infection, scarring and even spread of the wart. It’s best to leave wart removal to the professionals.
Myth 7: All Plantar Wart Removal Treatments Are the Same
There are several effective treatments for plantar warts, and the best option for you will depend on the size, location and number of warts. Options include:
- Cryotherapy: Freezing the wart with liquid nitrogen
- Laser therapy: Using a laser to destroy the wart
- Surgical removal: Cutting out the wart
- Topical medications: Applying prescription-strength creams or solutions
Effective Plantar Wart Removal in Singapore
If you’re struggling with plantar warts, seeking professional help is essential. A podiatrist can accurately diagnose the problem and recommend the most appropriate treatment for your specific situation. By understanding the facts about plantar wart removal, you can make better informed decisions about your treatment options and enjoy healthier, happier feet.
Say Goodbye to Plantar Warts with Straits Podiatry
Don’t let plantar warts disrupt your life. If you’re dealing with these stubborn growths, it’s time to seek professional help. Straits Podiatry offers evidence-based and safe plantar wart removal treatments in Singapore. Our experienced podiatrists can accurately diagnose your condition and recommend the best treatment.
Take the first step towards clear and healthy feet by contacting Straits Podiatry today. We’re committed to providing top-quality plantar wart removal services and helping you achieve foot wellness.
Jangkitan kulat kuku boleh menjadi masalah yang mengecewakan dan tidak sedap dipandang. Dicirikan oleh kuku yang berubah warna, menebal dan sering rapuh, jangkitan ini boleh menjejaskan kedua-dua kuku kaki dan kuku. Mengguna pakai beberapa tabiat penting dan perubahan gaya hidup boleh mengurangkan risiko anda mendapat jangkitan kulat kuku dengan ketara, menghapuskan keperluan untuk rawatan kulat kuku di kemudian hari.
Petua 1: Kekalkan Kebersihan Kuku yang Baik
Memastikan kuku anda bersih dan kering adalah asas dalam mencegah jangkitan kulat kuku. Bakteria dan kulat tumbuh subur dalam persekitaran yang lembap dan gelap, jadi memastikan kuku anda sentiasa bersih dan kering adalah penting.
Sentiasa potong dan kikir kuku anda dengan kerap, kerana kuku pendek kurang berkemungkinan memerangkap kotoran dan lembapan. Menggunakan kikir kuku yang bersih untuk melicinkan tepi kasar juga boleh membantu mengelakkan kecederaan. Paling penting, jangan kongsi alat penjagaan kuku seperti gunting kuku atau fail kerana ia boleh menyebarkan jangkitan.
Petua 2: Pakai Kasut yang Sesuai
Jenis kasut yang anda pakai boleh memberi kesan ketara kepada kesihatan kuku anda. Memilih kasut bernafas yang diperbuat daripada bahan seperti kulit atau kanvas membolehkan aliran udara yang lebih baik daripada bahan sintetik, membolehkan kaki anda bernafas, mengurangkan pengumpulan peluh dan lembapan.
Ingat bahawa stokin lembap mewujudkan tempat pembiakan kulat kuku. Oleh itu, tukar mereka setiap hari, terutamanya selepas aktiviti fizikal.
Petua 3: Elakkan Trauma Kuku
Kecederaan pada kuku anda boleh meningkatkan risiko jangkitan kulat kuku. Dengan mengambil langkah berjaga-jaga, anda boleh melindungi kuku anda daripada bahaya.
Ini bermakna mengelak daripada membenturkan kuku anda pada objek untuk mengelakkan lebam dan menggunakan alat dan teknik yang betul untuk membantu mencegah kuku tumbuh ke dalam, punca jangkitan yang biasa.
Petua 4: Tingkatkan Imuniti Keseluruhan Anda
Sistem imun yang kuat boleh membantu badan anda melawan jangkitan, termasuk jangkitan kulat kuku. Mengguna pakai gaya hidup sihat boleh meningkatkan fungsi imun anda. Anda harus sentiasa makan makanan seimbang untuk mendapatkan nutrien daripada pelbagai makanan, bersenam secara teratur dan tidur yang mencukupi yang penting untuk kesejahteraan keseluruhan dan fungsi imun.
Petua 5: Berhati-hati dengan Kawasan Awam
Tempat awam seperti kolam renang, gim dan pancuran mandian komunal boleh menampung kulat. Mengambil langkah berjaga-jaga seperti memakai selipar dan membersihkan kaki anda selepas terdedah kepada kawasan awam boleh membantu menghilangkan bakteria yang berpotensi dan membantu melindungi kuku anda.
Petua 6: Dapatkan Rawatan Kulat Kuku Profesional Awal
Jika anda mengesyaki jangkitan kulat kuku, adalah penting untuk mendapatkan rawatan kulat kuku profesional dengan segera. Campur tangan awal boleh menghalang penyakit daripada merebak dan menjadi lebih teruk. Pakar kaki atau doktor boleh mendiagnosis jangkitan dan mengesyorkan rawatan yang sesuai.
Lindungi kuku anda, cegah masalah
Memasukkan enam petua pencegahan ini ke dalam rutin harian anda boleh mengurangkan risiko anda mendapat jangkitan kulat kuku yang degil dengan ketara. Ingat, pencegahan sentiasa lebih baik daripada mengubati. Pengesanan dan rawatan awal adalah penting untuk menguruskan jangkitan kulat kuku dengan berkesan.
Jika anda bimbang tentang kesihatan kuku anda atau mengesyaki jangkitan kulat, jangan teragak-agak untuk mendapatkan nasihat profesional. Straits Podiatry menawarkan rawatan kulat kuku pakar dan boleh memberikan bimbingan peribadi untuk mencapai kuku yang sihat. Kawal kesihatan kuku anda hari ini dan nikmati keyakinan mempunyai kuku yang cantik dan menarik.
Amputations that are caused by diabetes are the ultimate fear for diabetic patients and healthcare professionals. The loss of a limb is a devastating outcome, but it can be preventable with diligent management and proactive care.
In this article, we will provide practical tips and strategies for preventing diabetes-related amputations and reducing your risk of this debilitating outcome.
The risk of diabetes-related amputations
Amputations in diabetic patients most commonly occur in the lower extremities, such as the toes, feet, and legs. Approximately 80% of these amputations are preceded by foot ulcers, which can result from even minor injuries that fail to heal properly due to poor blood circulation and nerve damage.
Here are some key numbers about diabetes-related amputations:
- Around 9 in 10 persons who had a lower limb amputation in Singapore had diabetes. [1]
- Estimated up to 4 diabetes-related amputations are performed every day in Singapore. [2]
- People with diabetes are up to 25 times more likely to undergo an amputation than those without diabetes. [3]
- More than 80% of lower-limb amputations in diabetic patients start with foot ulcers. [4]

How to prevent diabetes-related amputations?
The prevention of amputations requires a holistic approach that includes managing blood sugar levels, maintaining proper foot care, and seeking immediate medical attention for any foot issues.
Manage blood sugar levels
Make sure to keep your blood sugar levels within the target range to prevent complications that precipitate amputations. Chronically elevated blood sugar levels can damage blood vessels and nerves, reducing sensation and poor circulation in the feet.
Here are some strategies to help you with blood sugar management:
- Eat a balanced diet rich in vegetables, whole grains, and lean proteins. Also, avoid the consumption of excessive sugar and refined carbohydrates.
- Try to become physically active, which is great for blood circulation, weight loss, and blood sugar levels.
- Take your prescribed medications as directed by your healthcare provider compliantly (e.g., insulin, oral hypoglycemics).
- Monitor your blood glucose levels regularly to make sure that they remain within the normal range.
Incorporate foot care into your daily routine
Daily foot care is one of the most effective ways to prevent ulcers and amputations. A simple but consistent routine can identify potential problems before they become severe.
Follow these strategies:
Inspect your feet daily
Check your feet daily for cuts, blisters, redness, and swelling. Use a mirror to view the bottoms of your feet or ask for assistance if needed.
Wash and moisturize
Wash your feet daily with lukewarm water and mild soap. After that, dry them thoroughly, especially between the toes. Apply a moisturizer to keep the skin soft, but avoid applying lotion between the toes to prevent fungal infections.

Toenail care
Trim your toenails straight across and file any sharp edges. This prevents ingrown toenails.
Wear proper footwear
Choose shoes that fit well and provide adequate support. Avoid tight shoes and high heels, which cause blisters and sores. Always wear clean, dry socks, and avoid those with tight elastic bands.
Do not do the following!
Certain practices can increase the risk of foot injuries and ulcers, which can ultimately cause amputation.
First of all, do not go barefoot. This seemingly benign practice increases the risk of cuts, scrapes, and injuries that you might not feel due to peripheral neuropathy.
Secondly, avoid home remedies for foot lesions. Do not attempt to remove any corns and calluses, or other foot lesions yourself. Do not apply corn plasters or salicylic acid on any thickened skin areas. Instead, seek professional care from a podiatrist to avoid injury or infection.
Get regular medical checkups
Regular visits to your healthcare provider or podiatrist are essential to monitor your foot and catch any issues early on.
If you have diabetes, you need to have your feet examined by a healthcare professional at least once a year. However, if you have a history of foot ulcers, you need to get examined 2-4 times a year.
Finally, seek medical attention immediately when you notice any signs of diabetic foot infection. These signs may seem benign at first (e.g., redness, warmth, swelling), but they can worsen quickly. Early intervention can save your limb or even your life
Quit smoking
We know you have heard this a thousand times, but that should tell you something. Smoking significantly increases the risk of amputations in people with diabetes, according to a 2017 study. [5]
Chronic smoking impairs blood circulation and triggers low-grade inflammation, which contributes to the development of corns, calluses, and foot ulcers.

Perlukan Bantuan? Jumpa Pakar Podiat Kami Hari Ini
Stay on the look for foot ulcers
Diabetic foot ulcers are open sores or wounds that fail to heal properly due to poor blood circulation and nerve damage. They are a significant precursor to amputations, which makes their prevention and early treatment critical.
Signs of foot ulcers are:
- An ulcer that lasts longer than one to two weeks.
- Any ulcer that does not heal or worsen.
- An ulcer larger than 3/4 inch in diameter.
- An ulcer that is deep enough to expose the bone.
If you notice any of these signs, seek medical attention immediately.
Learn how to detect a foot ulcer early in this article.
The table below summarizes some key preventive measures for diabetes-related amputation:
| Preventive measure | Description |
| Blood sugar control | Maintain blood glucose levels within the target range. |
| Daily foot care | Inspect feet daily, wash, moisturize, and wear proper footwear. |
| Regular medical checkups | Annual foot exams and immediate care for any foot issues. |
| Smoking cessation | Quit smoking to improve circulation. |
| Healthy lifestyle | Manage your weight and blood pressure. |
| Diabetic foot team | Procedures to debride foot ulcers, control infection, and restore blood flow for adequate healing. |
How can a diabetic foot team prevent amputation?
One key evidence-based strategy to manage foot ulcers and prevent amputations is having a multidisciplinary care team. A team with various specialists, such as podiatrists, orthopaedic surgeons, and vascular surgeons, can provide well-coordinated holistic care.
For example, an individual with a severely infected diabetic foot ulcer may require an orthopaedic surgeon to remove dead infected tissues surgically. For individuals with severe PAD or diabetic foot ulcers, vascular surgery may be necessary to improve blood flow and prevent amputation. A podiatrist can then manage the wound through regular debridement and offloading to ensure the wound heals completely and prevents recurrence.
You can learn more about the benefits of multidisciplinary management of diabetic foot ulcers in this article.
Multidisciplinary Diabetic Foot Team
At Straits Podiatry, we have a dedicated diabetic foot care team that works closely with orthopaedic surgeons and other specialists to provide holistic management of any diabetic foot complications. Our goal is to ensure that you are seen quickly and have a tailored and coordinated management plan, so that we can minimise the risk of amputations.
If you suspect that you may have a diabetic foot ulcer or a non-healing wound, contact us or schedule an appointment today.
Mesej bawa pulang
Diabetes-related amputation is a life-altering complication that can be prevented when proper measures are put in place. Remember, vigilance and a commitment to foot care are key to prevention. Regular checkups, a healthy lifestyle, and smoking cessation are all critical components of an effective prevention strategy.
Rujukan
- https://www.niddk.nih.gov/health-information/professionals/diabetes-discoveries-practice/reducing-disparities-in-diabetic-amputations
- https://corp.nhg.com.sg/Media%20Releases/LEA%20Singapore_FINAL_edited.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10543925/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8316286/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5774386/
Pakar kaki berpengalaman dalam pengurusan kaki diabetes dan pencegahan amputasi.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
One of the most effective strategies for managing diabetic foot ulcers is implementing a multidisciplinary approach, which involves coordinated care from various healthcare professionals.
This approach has been shown to:
- Improve patient outcomes significantly.
- Reduce the incidence of amputations.
- Enhance the quality of care that is provided to diabetic patients.
In this article, we will list the benefits of adopting a multidisciplinary approach to diabetic foot ulcer treatment and review a case study that discusses this matter in detail.
Diabetic foot ulcers – An overview
The treatment of diabetic foot ulcers is complex as these ulcers commonly result from multiple factors. For instance, peripheral neuropathy affects up to 50% of diabetic patients, which reduces sensation in the feet and causes unnoticed injuries and ulcers. [1]
On the other hand, peripheral artery disease limits blood flow to the extremities, which obstructs the healing process and increases the risk of infection.
Aside from these factors, immunosuppression makes patients more susceptible to infections that can quickly escalate and result in sepsis. Keep in mind that most patients who live with diabetes for a long period of time are relatively immunocompromised (weakened immune system). [2]
The benefits of a multidisciplinary approach
A multi-disciplinary approach to diabetic foot ulcer treatment involves the collaboration of various specialists, including podiatrists, orthopaedic surgeons, vascular surgeons, plastic surgeons, endocrinologists, infectious disease specialists, physiotherapists, and diabetes educators.
This ensures that all aspects of the patient’s condition are addressed, which improves outcomes and significantly reduces the risk of severe complications.
1. Reduces the risk of amputations
One of the most significant benefits of a multidisciplinary approach is improving healing rates and reducing amputations. Studies have demonstrated that implementing a multidisciplinary team can decrease the incidence of major amputations.
For instance, a review of 33 studies found that 94% of the studies reported a reduction in major amputations (i.e. below-knee amputation) after establishing a multidisciplinary team. [3]
The comprehensive care these teams provide ensures that all contributing factors, such as diabetes control, local wound management, vascular disease, and infection, are addressed promptly and coordinated.
In a recent study that investigated the clinical benefits of adopting a multidisciplinary approach in managing diabetic foot ulcers, researchers found that the outcomes of patients are further improved when ortho-plastic surgery (a combination of orthopaedic and plastic surgeries) is incorporated. [4]
Here are the findings of this study:
- Team effort: The treatment of diabetic foot wounds effectively requires a team of specialists, including reconstructive surgeons, who play a critical role in the prevention of amputations.
- Limb salvage: The approach prioritizes limb preservation over amputation and addresses all aspects of the condition. This includes blood flow issues, infections, and the correction of any foot deformities.
- Better quality of life: The use of these combined methods benefits patients by allowing them to maintain mobility and improve their quality of life. They also lower the incidence of complications and the risk of recurrences.
- Complexity and customisation: Each case is complex and requires tailored treatments that include careful management of blood sugar levels, proper wound care, and strategic surgical and non-surgical interventions that consider the entire foot’s condition.
2. Provides coordinated care
The coordinated care provided by the multidisciplinary approach is extremely valuable. Timely interventions can prevent the progression of ulcers and lower the need for amputations. This is one of the key factors that makes such an approach so effective.
Here’s the specific role of each specialist:
- Regular assessments, wound debridement, and offloading by a podiatrist to manage the foot ulcer.
- Vascular surgeons will assess your feet to ensure adequate blood flow.
- Adjustments in diabetes medications by an endocrinologist to maintain optimal blood glucose levels.
- In cases where infection is present, an infectious disease specialist can provide targeted antibiotic therapy to control the infection and prevent its spread.
3. Educate the patient about their condition
Patient education is another central element of the multidisciplinary approach. Healthcare professionals will teach patients about proper foot care, the importance of glycemic control, and the early signs of foot complications. This can significantly reduce the risk of developing foot ulcers.
You can learn how to detect a potential foot ulcer in this article.
The role of technology in the multidisciplinary approach to foot ulcer treatment
It’s true that the success of a multidisciplinary approach largely depends on the expertise and collaboration of the team members. However, the appropriate tools and technology can also significantly improve patient outcomes.
For example, advanced wound care products, such as negative pressure wound therapy and specialized dressings, promote faster healing and reduce the risk of infection.
Perlukan Bantuan? Jumpa Pakar Podiat Kami Hari Ini
A case study
A retrospective cohort study conducted at the Gosford Hospital High-Risk Foot Clinic in Australia provides a clear example of the benefits of a multi-disciplinary approach to diabetic foot ulcer management. [5]
The study compared patient outcomes before and after implementing a multidisciplinary team. The results showed a significant reduction in the median time to ulcer healing, from 20.4 weeks in 2017 to 14.2 weeks in 2019.
Additionally, the percentage of ulcers that healed within 52 weeks had increased by 10.1%. The number of vascular interventions had also increased by 17.4%, which shows how this approach effectively identifies at-risk patients early and manages them before they worsen.
The table below showcases the significant improvements in patient outcomes after the implementation of a multi-disciplinary team (MDT). [5]
| Outcome | 2017 (before MDT) | 2019 (after MDT) |
| Median time to ulcer healing | 20.4 weeks | 14.2 weeks |
| Percentage of ulcers that healed | 58% | 68% |
| Incidence of vascular interventions | 1.6% | 19% |
Mesej bawa pulang
Due to the complexity of the condition and the multiple factors contributing to its development and progression, the treatment of diabetic foot ulcers requires a comprehensive and coordinated approach. A multidisciplinary approach involves collaboration between various specialists to improve patient outcomes, reduce the risk of amputations, and enhance the quality of care.
Pasukan Kaki Diabetes Pelbagai Disiplin di Singapura
At Straits Podiatry, we understand the importance of adopting a multidisciplinary approach to managing diabetic foot complications. Therefore, we have a well-coordinated diabetic foot team of podiatrists, orthopaedic surgeons, and other specialists who strive to provide you with efficient, tailored care.
We hope this article helped you appreciate the significant role of a multidisciplinary approach in diabetic foot treatment.
If you suspect that you may have a diabetic foot ulcer, schedule an appointment with our diabetic foot team today.
If you have any questions about our multidisciplinary approach to diabetic foot management, feel free to check out via this link (insert).
Rujukan
- https://emedicine.medscape.com/article/1170337-overview
- https://pubmed.ncbi.nlm.nih.gov/31657690/
- https://www.researchgate.net/publication/336993156_A_systematic_review_of_multidisciplinary_ teams_to_reduce_major_amputations_for_patients_with_diabetic_foot_ulcers
- https://www.sciencedirect.com/science/article/pii/S2666769X24000010
- https://pubmed.ncbi.nlm.nih.gov/38379247/
Pakar kaki berpengalaman dalam pengurusan kaki diabetes dan pencegahan amputasi.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Knee pain can be a real bother, making everyday activities a challenge. Consider seeing a knee specialist in Singapore if you’re experiencing knee discomfort. These experts can provide the care and expertise needed to get you back on your feet.
Understanding Knee Pain and the Importance of Early Intervention
Your knee is a complex joint that supports your weight and allows movement. Experiencing knee pain indicates that something is amiss. Common causes of knee pain include arthritis, injuries and overuse.
Overlooking knee pain can lead to complications, and delaying treatment may result in more severe issues and a prolonged recovery. Early intervention is crucial for effective knee pain treatment in Singapore. A knee specialist can accurately diagnose the problem and recommend appropriate treatment to prevent further damage.
Benefits of Seeing a Knee Specialist in Singapore
Knee pain can bring many inconveniences to your daily life. Seeking the expertise of a knee specialist in Singapore offers numerous advantages for effective knee pain treatment.
Accurate Diagnosis
Knee pain can stem from various underlying causes. A knee specialist possesses the in-depth knowledge and experience to accurately diagnose the root of your knee problem. Through a comprehensive evaluation, including physical examinations and diagnostic imaging, they can identify the specific condition affecting your knee. This precision is crucial for developing an appropriate treatment plan.
Tailored Treatment Plans
Knee specialists understand that every patient is unique. They create personalised treatment plans that consider your specific condition, medical history, lifestyle and goals. This tailored approach ensures you receive the most effective and suitable knee pain treatment for your individual needs.
Access to Advanced Treatment Options
Singapore is renowned for its cutting-edge medical advancements. Knee specialists in Singapore have access to the latest treatment options, including minimally invasive procedures, advanced therapies and rehabilitation techniques. This means you can benefit from the most up-to-date and effective treatments available for your knee pain.
Comprehensive Care
A knee specialist provides comprehensive care, addressing the physical aspects of your condition and its impact on your daily life and emotional state. They work with you to develop a holistic knee pain treatment plan promoting your health and well-being.
Prevention of Long-Term Issues
Early intervention is key to preventing knee pain from progressing into chronic conditions. A knee specialist can identify potential risks and implement preventive measures to protect your knee joint and avoid the need for more complex treatments in the future.
Pemulihan Lebih Cepat
Knee specialists have the expertise to develop efficient treatment plans and provide appropriate guidance to facilitate a quicker recovery from knee pain. They can help you regain mobility, strength and function quickly, allowing you to return to normal activities and enjoy life without limitations.
Peace of Mind
Knowing you are under the care of a qualified knee specialist can provide significant peace of mind. Their expertise and support can alleviate anxiety and concerns related to your knee pain, empowering you to take control of your recovery process.
By seeing a knee specialist in Singapore, you can access specialised care, advanced treatment options and a comprehensive approach to managing your knee pain.
Take the First Step Towards a Pain-Free Life
Don’t let knee pain hinder your daily activities and quality of life. If you’re experiencing knee discomfort, seeking the expertise of a knee specialist in Singapore is a crucial step towards effective treatment and long-term relief.
At Straits Podiatry, our dedicated team of podiatrist is committed to providing comprehensive care and personalised treatment plans to address your unique needs. With our advanced facilities and expertise in knee pain treatment in Singapore, we are dedicated to helping you regain mobility, strength and confidence.
Remember, early intervention is key to preventing further complications. Don’t hesitate to seek professional help from a qualified knee specialist. Contact Straits Podiatry today to schedule a consultation and take the first step towards a life without knee pain!
Memahami Sakit Tumit
Plantar fasciitis is a common foot condition that causes heel pain. It happens when the plantar fascia, a thick band of tissue on the bottom of your foot, becomes inflamed and irritated. Walking, standing, or even getting out of bed in the morning can make it painful. If you’re experiencing heel pain, you’re not alone, and finding the proper heel pain treatment is critical to getting relief.

The Role of Shoes in Plantar Fasciitis Treatment
Choosing the right shoes is one of the most essential steps in treating plantar fasciitis. Your footwear is crucial in supporting your feet and reducing heel pain. Good shoes can help absorb shock, provide proper arch support, and align your feet correctly.
Key Features to Look for in Plantar Fasciitis Shoes
Choosing the right shoes for plantar fasciitis treatment in Singapore is essential for relieving heel pain. Look for shoes with these key features:
Arch Support
Good arch support is crucial for plantar fasciitis treatment. It helps distribute your weight evenly across your foot, reducing the strain on your plantar fascia. Look for shoes with a contoured insole for arch support built into the sole. This will help to cradle your foot and provide the necessary support for your heel pain.
Cushioning
Cushioning is another important factor to consider when choosing shoes for plantar fasciitis. Good cushioning absorbs shock and reduces impact on your heel, helping to alleviate pain. Look for shoes with plenty of cushioning in the heel and forefoot area. This will provide comfort and support throughout the day.
Heel Support
Proper heel support is essential for stabilising your foot and ankle. It helps to prevent excessive motion and reduce stress on the plantar fascia. Look for shoes with a deep heel cup that securely holds your heel. This will help to relieve heel pain and prevent further irritation.
Flexibility
While your shoes need to provide support, they should also be flexible enough to allow for natural foot movement. Look for shoes with a flexible sole that bends with your foot. This will help to promote proper foot function and reduce discomfort.
Motion Control
You may benefit from shoes with motion control features if you have overpronation or supination (flat feet or high arches). These shoes help to correct abnormal foot movement and reduce strain on the plantar fascia. If you’re unsure about your foot type, it’s best to consult a podiatrist for advice.
Finding the Right Shoes in Singapore
With so many shoe options in Singapore, finding the perfect pair for plantar fasciitis treatment can be challenging. Here are some tips to help you find the right shoes:
Try Before You Buy
It’s essential to try on shoes before buying them to ensure a proper fit. Your feet can swell throughout the day, so it’s best to try on shoes in the afternoon when they are at their largest. Try different styles and brands to find the shoes that offer the best support and comfort for your feet.
Consider Orthotic Inserts
Orthotic inserts may be beneficial if you still experience heel pain despite wearing supportive shoes. Orthotics are custom-made shoe inserts that provide additional arch support and cushioning. They can help to alleviate plantar fasciitis symptoms and improve overall foot comfort.
Seek Professional Advice
If you need help finding the right shoes, consider consulting with a Singapore-based podiatrist or specialist shoe store. They can assess your feet, recommend suitable shoe styles, and provide personalised advice on plantar fasciitis treatment.
Your Journey to Heel Pain Relief Starts Here
Finding the right shoes is crucial in managing plantar fasciitis and reducing heel pain. By understanding the key features to look for and taking the time to find the perfect fit to support your feet, you can significantly improve your comfort and overall well-being. Remember, every foot is unique, so it’s essential to prioritise comfort and support when choosing your footwear.
If you’re still experiencing heel pain despite trying different shoes, it’s time to seek professional help. Straits Podiatry offers expert care for plantar fasciitis treatment in Singapore. Our experienced podiatrists can diagnose your condition, recommend appropriate treatment options and provide personalised guidance to help you find relief from heel pain.
Don’t let plantar fasciitis hinder your daily activities. Take the first step towards a pain-free life by contacting Straits Podiatry today.
Ankle injuries are common for many people, from sports enthusiasts to everyday walkers. Whether it’s a sprain, strain or fracture, dealing with ankle injuries can be frustrating and disruptive to your daily life. The good news is that with proper care and a balanced approach, you can effectively recover and get back on your feet.
Understanding Ankle Injuries
Before diving into the recovery process, it’s essential to understand the different types of ankle injuries. Ankle sprains are the most common, occurring when the ligaments supporting the ankle joint are stretched or torn. Ankle strains involve damage to the muscles or tendons around the ankle, while fractures are breaks in the ankle bones.
Early and accurate diagnosis is crucial for effective ankle injuries treatment. Ignoring or mishandling ankle injuries can lead to complications, including chronic pain, instability and even arthritis.
The Crucial Role of Rest in Ankle Injuries Treatment
When it comes to healing ankle injuries, rest is paramount. The initial stages of recovery require complete rest to allow the injured tissues time to repair. Your doctor might recommend using an ankle brace or boot to immobilise the joint and prevent further damage.
While resting is essential, managing discomfort and pain effectively is significant. Over-the-counter pain relievers, ice packs and elevation can help alleviate symptoms in the early stages.
The Benefits of Controlled Activity for Ankle Injury Recovery
While rest is crucial for the initial healing of ankle injuries, it’s equally important to gradually introduce controlled activity into your recovery plan. Explore the advantages of regulated activity and how it can positively impact your ankle injuries treatment.
Improve Blood Circulation
Engaging in gentle movement helps increase blood flow to the injured area. This delivers essential nutrients and oxygen, accelerating healing and reducing swelling.
Prevent Stiffness and Muscle Atrophy
Prolonged inactivity can lead to stiffness and muscle weakness in the ankle and surrounding areas. Controlled activity helps maintain flexibility and strength, preventing further complications.
Pemulihan Lebih Cepat
Incorporating suitable exercises into your routine can expedite healing and allow you to return to normal activities sooner.
Boost Mental Health
Physical activity is known to improve mood, reduce stress and combat feelings of isolation often associated with injuries.
Safe and Effective Exercises for Ankle Injuries Treatment
Once your doctor approves, it’s time to rebuild your ankle’s strength and flexibility. Focus on low-impact exercises that target the ankle joint and surrounding muscles. Here are some examples:
Ankle Circles
Gently rotate your ankle clockwise and counterclockwise to improve your range of motion.
Calf Stretches
Stand facing a wall, place your hands on the wall for support, and gently lean forward while keeping your heel flat on the ground to stretch your calf muscles.
Heel Raises
Stand with your feet shoulder-width apart and slowly rise onto your toes, then lower back down. This exercise helps strengthen the calf muscles.
Balance Exercises
Practice standing on one leg for short periods to improve balance and ankle stability.
Remember to listen to your body and gradually increase the intensity and duration of your exercises. If you experience any pain, stop and rest.
Alternative Activities to Stay Active During Recovery
While focused ankle exercises are essential, incorporating other activities into your routine can help maintain overall fitness and prevent boredom. Here are some options:
Swimming
This low-impact exercise allows you to move your body without putting weight on your ankle. It provides a full-body workout while being gentle on the injured joint.
Cycling (Stationary Bike)
Stationary cycling is a great way to exercise your legs without straining your ankle. It can help improve cardiovascular health and lower body strength.
Upper Body Workouts
Focus on exercises that target your arms, shoulders and core to maintain overall fitness while your ankle heals.
Yoga or Pilates
These practices incorporate gentle movements, stretching and breathing exercises to improve flexibility, balance and core strength.
Remember to choose activities that are enjoyable and suitable for your fitness level. Always consult with your healthcare professional before starting any new exercise regimen.
Preventing Ankle Re-injury
Preventing ankle re-injury is crucial for long-term well-being. Proper footwear with good ankle support can significantly reduce the risk of future ankle injuries. Continuing ankle strengthening exercises can help maintain ankle stability and resilience even after complete recovery.
Furthermore, maintaining a healthy weight can alleviate stress on the ankle joints, reducing the likelihood of re-injury.
Your Journey to Ankle Injury Recovery
Balancing rest and controlled activity is essential for optimal ankle injuries treatment and recovery. While the initial focus should be resting the injured ankle, gradually incorporating specific exercises and alternative activities can significantly speed up healing. Remember, patience and consistency are critical to a successful recovery.
If you’re dealing with an ankle injury and need expert guidance, Straits Podiatry is here to help. Our team of experienced podiatrists can provide comprehensive ankle injuries treatment, including diagnosis, rehabilitation and preventive care. Contact us today to schedule a consultation and take the first step towards a full recovery.
Diabetic foot ulcer is a common and serious complication that occurs in diabetic patients. It affects up to 15% of patients. Unfortunately, more than 50% of individuals with these ulcers may face life-threatening complications within five years if left untreated. [1][2]
Recognizing the early signs of a foot ulcer is critical because rapid intervention can prevent amputations.
In this article, we will discuss signs and symptoms that can help you identify if you have a diabetic foot ulcer early on.
The Signs and Symptoms of Diabetic Foot Ulcers
Here are the main symptoms to be aware of:
Perubahan warna kulit
One of the first indicators of a foot ulcer is a noticeable change in skin colour. This may include redness, darkening, or a bluish tint around the affected area.
Discoloration is due to inflammation and compromised blood flow to the tissues, which signals the early stages of an ulcer.
Swelling and redness
Swelling around a specific area on your foot can also indicate the onset of an ulcer, especially if it’s associated with redness. This swelling may extend to surrounding tissues and should be monitored closely.
Presence of calluses or corns
Calluses and corns are thickened areas of skin that result from repeated friction or pressure. Although they are prevalent in people with diabetes, they can also be precursors to foot ulcers. If left untreated, they may develop into open sores or wounds.
Pain and tenderness
Although peripheral neuropathy might reduce the sensation in your feet, you may still experience some pain or tenderness. This could be a sign of underlying tissue damage or the early stages of a foot ulcer.
Drainage and odour
If you notice any unusual drainage from a wound on your foot with a pungent odour, this could be a sign of infection.
It’s important to seek medical attention immediately if you observe these symptoms.

Visual characteristics of diabetic foot ulcers
Foot ulcers can vary in appearance. However, there are common visual cues that can help you identify them:
Size and shape of the ulcer
Foot ulcers can range in size from small and round sores to larger and irregularly shaped wounds. Early-stage ulcers might be less than a centimeter in diameter and may seem minor, but they should never be ignored.
As ulcers progress, they can become deeper and more severe, which exposes subcutaneous (fatty) tissues, muscles, joints and even bones.
Surrounding skin condition
The skin around a foot ulcer might be thickened, dry, or callused. In more advanced stages, the ulcer could be surrounded by eschar (a black or brown tissue that forms due to necrosis—tissue death). Eschar is a serious sign that requires immediate medical intervention.
Depth and tissue involvement
The depth of the ulcer can provide insight into its severity. Superficial ulcers involve only the skin, whereas deeper ulcers may affect underlying tissues. The deeper the ulcer, the greater the risk of complications (e.g. infections).
How to prevent diabetic foot ulcers
The prevention of diabetic foot ulcers is the best approach, as management can be very complicated.
Here are some practical steps you can take:
Maintain proper blood sugar levels
Keep your blood sugar levels under control to prevent diabetes complications. According to studies, this is one of the most effective ways to prevent foot ulcers. What’s more, a healthy diet, proper compliance with treatment, and regular physical activity can all prevent diabetic foot ulcers. [3]
Regular foot care routine
Incorporate daily foot care into your routine. This includes washing your feet with warm water and mild soap, drying them thoroughly (especially between the toes), and inspecting them for any cuts, sores, or changes in colour. You should also moisturise your feet daily and gently file any dry, thickened skin.
Make sure to use a mirror to check areas that are difficult to see.
Choose appropriate footwear
Wear well-fitting shoes that protect your feet from injury. Avoid tight shoes as they can cause blisters or sores that may develop into ulcers. You should also always wear slippers at home, preferably those with thick, soft soles and covers the toes to protect your feet from any accidental cuts.
Also, consider putting on socks that provide cushioning and reduce friction.
Trim your nails carefully
After bathing, trim your nails straight across to avoid ingrown toenails, which can cause infections. Filing rough edges can also prevent skin damage.
Avoid prolonged pressure
Try not to sit, stand, or cross your legs for extended periods. These habits can impede blood flow to your feet and cause pressure sores. Proper circulation is indispensable for healing wounds and preventing ulcers.

When to Seek Medical Attention
Diabetic foot ulcers are serious and require prompt medical attention. Here are the situations when you should see a healthcare professional:
If you notice any of the early signs mentioned—such as discolouration, swelling, or the presence of calluses or corns—schedule an appointment with a podiatrist or a diabetic foot specialist. Early intervention can prevent the ulcer from worsening and reduce the risk of amputations.
Don’t ignore ongoing pain, tenderness, or discomfort in your feet. These symptoms may indicate a developing ulcer or an existing one that requires more intensive care. If a wound on your foot does not show signs of healing after a few days of home care, it’s essential to consult with your doctor. Non-healing wounds are at high risk of infection and need professional treatment.
Symptoms like drainage, a foul odour, or the appearance of eschar around a wound are clear indicators of infection. In such cases, immediate medical care is necessary to prevent the infection from spreading and to avoid more severe outcomes, such as amputation.
Check out this article to learn more about diabetic foot ulcer treatment.
Pasukan Kaki Diabetes Pelbagai Disiplin di Singapura
At Straits Podiatry, we understand the importance of managing ulcers early to reduce the risk of amputations. Therefore, we have a diabetic foot team consisting of podiatrists, orthopaedic surgeons and other specialists who strive to provide multidisciplinary care that is efficient and tailored to your needs.
If you suspect that you may have a diabetic foot ulcer, contact us or schedule an appointment with our diabetic foot team today.
Perlukan Bantuan? Jumpa Pakar Podiat Kami Hari Ini
Mesej bawa pulang
Diabetic foot ulcers are a serious complication that requires vigilance, early diagnosis, and aggressive management. Understanding early signs and symptoms, visual characteristics of ulcers, and preventive measures can all reduce the risk of diabetic foot ulcers.
We hope this article sheds some light on how to tell when you develop a diabetic foot ulcer.
If you have any questions or concerns about diabetic foot ulcers, feel free to check out other posts that we covered.
Rujukan
Pakar kaki berpengalaman dalam pengurusan kaki diabetes dan pencegahan amputasi.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Bursitis tumit, termasuk bursitis retrocalcaneal, adalah keadaan biasa yang biasanya menjejaskan individu yang aktif secara fizikal. Ia menyebabkan kesakitan dan ketidakselesaan di bahagian belakang kawasan tumit. Kesakitan selalunya lebih teruk semasa dan selepas aktiviti fizikal, menjadikannya sukar untuk mengekalkan gaya hidup aktif. Jika ini terdengar seperti apa yang anda alami, baca sehingga akhir untuk memahami cara menguruskan bursitis tumit dengan berkesan.
Memahami Bursitis Tumit
Bursitis tumit pada asasnya ialah keradangan bursae, iaitu kantung kecil berisi cecair di antara tulang, tendon dan otot anda. Bursae membantu mengurangkan geseran antara struktur semasa pergerakan dan kesan kusyen. Kami mempunyai berbilang bursae di pelbagai lokasi kaki, dan anda mungkin berkembang lebih banyak di kawasan geseran yang tinggi.
The most common type of heel bursitis affecting the heel is retrocalcaneal bursitis, which occurs behind the heel where the Achilles tendon attaches to the heel bone (calcaneus). This condition can cause significant heel pain and swelling, particularly during activities that involve pressure on the heel. Movements such as incline walking, running, or jumping can make the pain worse. Some individuals also report pain when wearing shoes with stiff heel counters.
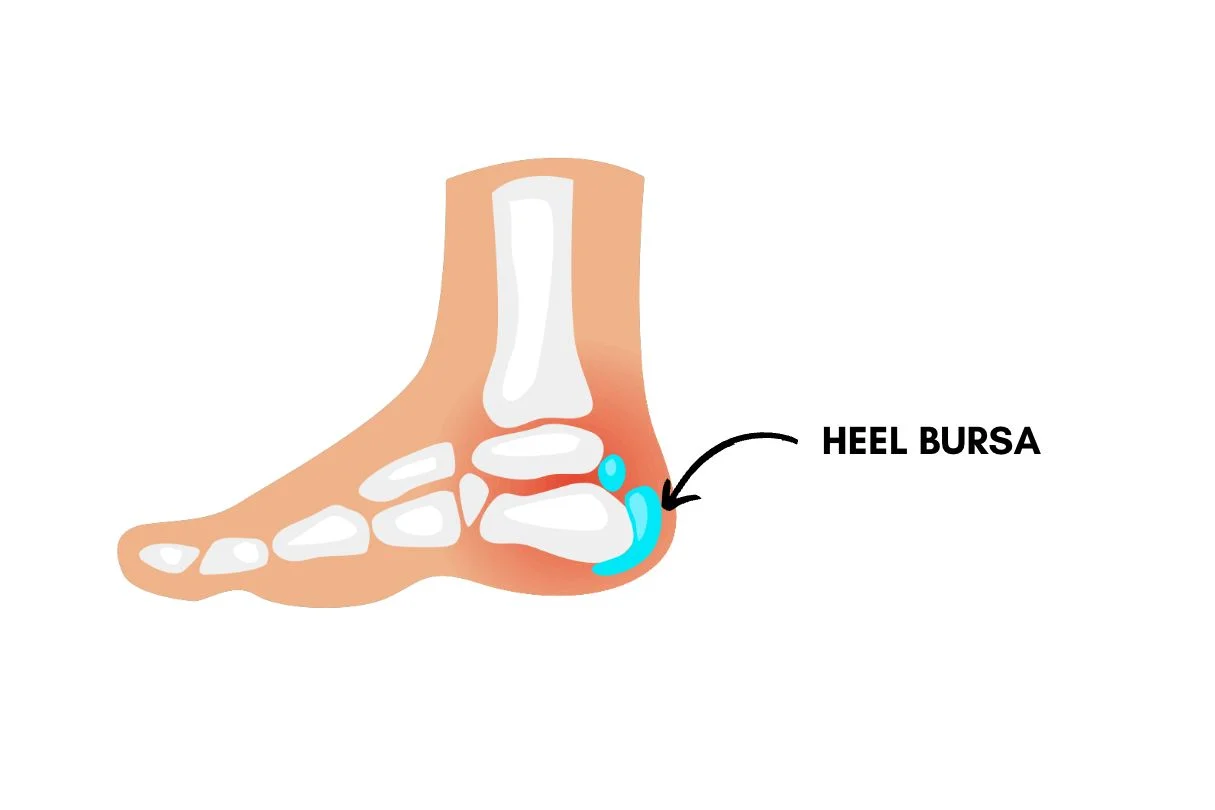
Punca Biasa Bursitis Tumit
Kecederaan Penggunaan Berlebihan
Tekanan berulang atau aktiviti berlebihan, seperti berlari atau melompat, boleh menimbulkan terlalu banyak geseran antara tendon Achilles dan tulang tumit, yang membawa kepada kerengsaan dan keradangan bursa.
Kasut yang tidak sesuai atau tidak betul
Kasut yang tidak memberikan sokongan yang mencukupi atau tidak sesuai boleh menyumbang kepada perkembangan bursitis tumit. Kasut yang terlalu kecil boleh memampatkan kawasan tumit, meningkatkan geseran. Anda juga perlu mengetahui kasut sukan tertentu di mana kaunter tumit condong ke dalam pada sudut senget, kerana itu juga akan meningkatkan tekanan di sekeliling bahagian belakang tumit.
Kecederaan atau Trauma
Trauma langsung boleh mencetuskan bursitis tumit atau bursitis retrocalcaneal. Kesan trauma langsung pada tumit boleh menyebabkan keradangan bursae, menyebabkan kemerahan, kesakitan, dan bengkak.
Keabnormalan Struktur Kaki
Struktur kaki sangat mempengaruhi corak berjalan atau berlari kita. Keabnormalan dalam struktur kaki boleh mengubah mekanik kaki dan meningkatkan tekanan pada otot, tendon, sendi dan tulang. Keadaan seperti gerbang tinggi atau kaki rata boleh meningkatkan tekanan antara tendon Achilles dan tulang tumit, mengakibatkan bursitis retrocalcaneal.
Keadaan Keradangan Sistemik
Systemic conditions such as rheumatoid arthritis or gout can trigger inflammation in the bursae. Heel bursitis caused by inflammatory conditions usually has a rapid onset and can be very painful, red, and swollen.
Gejala Bursitis Tumit
- Sakit: Sakit tajam atau sakit di bahagian belakang tumit, terutamanya dengan pergerakan atau tekanan.
- Kemerahan: Kelihatan merah di sekitar kawasan tumit, biasanya dengan peningkatan kehangatan.
- Bengkak: Bengkak yang ketara di sekitar kawasan tumit, terutamanya di bahagian belakang tulang tumit untuk bursitis retrocalcaneal.
- Kekakuan: Kesukaran menggerakkan kaki atau rasa kekakuan di tumit, terutamanya selepas tempoh rehat.

Pilihan Rawatan Bursitis Tumit di Singapura
Untuk menguruskan bursitis tumit atau bursitis retrocalcaneal dengan berkesan, anda mesti menangani kecederaan dan punca asas secara serentak. Faktor biasa yang perlu dipertimbangkan dan pilihan rawatan yang disyorkan ialah:
Pengurusan Kesakitan
- Rehat dan Ais: Langkah pertama selalunya melibatkan merehatkan kaki yang terjejas dan menggunakan ais dan mampatan untuk mengurangkan keradangan dan kesakitan.
- Ubat penahan sakit: Ubat anti-radang tanpa preskripsi atau ubat sakit juga boleh membantu mengurangkan kesakitan. Walau bagaimanapun, anda mesti faham bahawa anda tidak boleh mengambil ubat penahan sakit hanya untuk meneruskan aktiviti anda atau berisiko menyebabkan kerosakan selanjutnya.
Kasut dan Ortotik
- Appropriate Supportive Footwear: It is essential to select shoes that provide adequate support and cushioning to reduce pressure on the heel. Seeing a Podiatrist can help receive guidance in selecting the right pair for you.
- Custom Orthotics: Customised orthotic devices can help correct foot mechanics and alleviate stress on the bursa. This is particularly important if you have a high arch or flat feet.
Terapi Fizikal dan Pemulihan
- Pengubahsuaian Aktiviti: Kami amat mengesyorkan beralih kepada aktiviti berimpak rendah jika anda terlalu banyak memaksa. Contohnya ialah bertukar daripada berlari kepada berenang.
- Latihan Regangan dan Pengukuhan: Program pemulihan berpandu boleh membantu menguatkan otot di sekeliling tumit dan meningkatkan fleksibiliti, sekali gus mengurangkan ketegangan pada bursa.
Terapi Tisu Lembut Lanjutan
- Pelepasan Titik Pencetus: Teknik seperti gelombang tekanan jejari atau jarum kering boleh digunakan untuk melepaskan ketegangan dan meningkatkan fleksibiliti otot, terutamanya otot betis, dalam kes bursitis tumit.
- Terapi Gelombang Kejutan: Terapi gelombang kejutan ekstrakorporeal boleh membantu merangsang dan mempercepatkan proses penyembuhan semula jadi badan.
Intervensi Invasif Lain
Dalam kes yang jarang berlaku di mana rawatan konservatif tidak berkesan, profesional perubatan anda mungkin mengesyorkan suntikan untuk melegakan keradangan. Pilihan pembedahan jarang dipertimbangkan atau dilakukan untuk keadaan ini. Ini boleh melibatkan pembuangan bursa yang meradang atau menangani sebarang isu struktur yang mendasari, seperti ketegangan otot betis, yang menyumbang kepada keadaan.

Bagaimana untuk Mencegah Bursitis Tumit?
Untuk mengelakkan berulangnya bursitis tumit atau bursitis retrocalcaneal, anda harus ingat perkara berikut:
- Pakai Kasut Sokongan: Pilih kasut dengan sokongan tumit dan lengkungan yang betul dan kusyen untuk mengurangkan tekanan pada tumit.
- Pengurusan Beban: Berat badan atau beban yang berlebihan boleh meningkatkan tekanan pada kaki dan menyumbang kepada bursitis. Jangan terlalu memaksakan diri atau berisiko cedera.
- Lakukan Regangan Biasa: Senaman regangan untuk tendon Achilles dan otot betis boleh meningkatkan fleksibiliti dan membantu mengelakkan kekakuan dan ketegangan.
- Elakkan Penggunaan Berlebihan: Tingkatkan tahap aktiviti secara beransur-ansur dan elakkan senaman yang tiba-tiba dan sengit yang boleh menegangkan kaki.
Kesimpulan
Pengurusan bursitis tumit yang berkesan, termasuk bursitis retrocalcaneal, memerlukan pendekatan komprehensif yang disesuaikan dengan keperluan setiap individu. Keadaan ini jarang memerlukan kaedah invasif untuk mencapai kelegaan yang optimum.
Di Straits Podiatry, kami komited untuk menyediakan penjagaan podiatri berkualiti tinggi dan rawatan inovatif untuk membantu anda mengatasi bursitis tumit dan kembali kepada aktiviti biasa anda. Jika anda mengalami sakit tumit atau mengesyaki anda mungkin menghidap bursitis, jangan teragak-agak untuk menghubungi kami untuk penilaian dan pengurusan yang menyeluruh. Pasukan Pakar Podiatrik kami yang berpengalaman akan berusaha untuk membolehkan anda bangkit semula.
Soalan Lazim (Soalan Lazim) Mengenai Bursitis Tumit
1. Apakah perbezaan antara bursitis retrocalcaneal dan tendinitis Achilles?
Bursitis retrocalcaneal ialah keradangan bursa yang terletak di belakang tulang tumit di mana tendon Achilles melekat. Sebaliknya, tendinitis Achilles merujuk kepada keradangan atau degenerasi tendon Achilles itu sendiri. Kedua-dua keadaan boleh menyebabkan sakit tumit, tetapi ia melibatkan struktur yang berbeza dan mungkin memerlukan pendekatan rawatan yang berbeza.
2. Berapa lama masa yang diambil untuk pulih daripada bursitis tumit?
Masa pemulihan untuk bursitis tumit berbeza-beza bergantung kepada keterukan keadaan dan keberkesanan rawatan. Dengan pengurusan yang sesuai, ramai individu biasanya mengalami peningkatan dalam masa beberapa minggu. Walau bagaimanapun, pemulihan lengkap mungkin mengambil masa sehingga beberapa bulan, terutamanya jika keadaannya kronik atau teruk.
3. Bolehkah saya terus bersenam dengan bursitis tumit?
Apabila anda menghidap bursitis tumit, kami mengesyorkan mengubah suai rutin senaman anda untuk mengelakkan tekanan selanjutnya pada tumit dan kaki anda. Aktiviti berimpak rendah, seperti berenang atau berbasikal, adalah pilihan yang baik untuk menggantikan aktiviti berlari atau melompat. Berunding dengan pakar kaki untuk membangunkan pelan senaman yang menampung keadaan anda sambil menggalakkan penyembuhan.
4. Adakah terdapat sebarang ubat rumah yang boleh membantu dengan bursitis tumit?
Ya, terdapat beberapa pilihan ubat rumah yang boleh anda cuba, termasuk berehat dan aising untuk mengurangkan keradangan dan menggunakan ubat penahan sakit tanpa preskripsi. Memakai kasut yang betul dan melakukan senaman regangan lembut juga boleh membantu mengurangkan gejala. Walau bagaimanapun, adalah penting untuk berunding dengan pakar kaki jika anda tidak mendapat sebarang kelegaan.
5. Bilakah saya perlu berjumpa pakar kaki untuk bursitis tumit?
Anda harus berjumpa pakar kaki jika anda mengalami sakit tumit yang berterusan, bengkak atau ketidakselesaan yang tidak bertambah baik dengan rehat dan penjagaan di rumah. Pakar kaki boleh memberikan penilaian menyeluruh, diagnosis yang tepat dan pelan pengurusan yang diperibadikan untuk menangani keperluan khusus anda dan mencegah komplikasi selanjutnya.
Artikel Berkaitan:
- Anatomi tumit: memahami struktur kompleks
- Perubahan Gaya Hidup untuk Mencegah Sakit Tumit di Persekitaran Bandar Singapura
- Mengapa saya mengalami sakit tumit?
- Peranan Terapi Shockwave dalam Rawatan Fasciitis Plantar
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Di Singapura, trend mengamalkan gaya hidup sihat dan aktif semakin meningkat. Ramai pesakit kami telah memberitahu kami bahawa mereka cuba mencatat 10,000 langkah sehari dan 30 minit aktiviti fizikal sederhana seminggu. Walau bagaimanapun, dengan peningkatan aktiviti sedemikian, kecederaan boleh berlaku. Salah satu masalah biasa yang mungkin dihadapi ialah mengalami kesakitan di bahagian atas kaki anda. Kesakitan jenis ini boleh disebabkan oleh pelbagai sebab dan mungkin memerlukan pendekatan rawatan yang berbeza. Memahami sebab yang berpotensi di sebalik kesakitan di bahagian atas kaki anda boleh membantu anda mendapatkan penjagaan dan kelegaan yang sesuai dengan berkesan. Berikut ialah panduan komprehensif tentang punca biasa kesakitan di bahagian atas kaki.
Punca biasa kesakitan di bahagian atas kaki
Extensor Tendonitis
Tendon ekstensor terdiri daripada 3 otot utama: tibialis anterior, halusis longus ekstensor, dan digitorium longus ekstensor. Tendon ini berjalan di sepanjang bahagian atas kaki dan bertanggungjawab untuk mengangkat jari kaki dan kaki. Penggunaan berlebihan atau ketegangan yang berlebihan, selalunya daripada aktiviti seperti berlari atau melompat, boleh menyebabkan tendonitis ekstensor (keradangan). Ini mengakibatkan kesakitan, bengkak, dan kelembutan di sepanjang bahagian atas kaki, terutamanya apabila menggerakkan jari kaki atau kaki.
Ketegangan Tendon
Bentuk kecederaan tendon yang lebih ringan berbanding tendonitis, ketegangan pada tendon kaki, boleh berlaku disebabkan oleh aktiviti fizikal secara tiba-tiba atau sengit. Ketegangan tendon membawa kepada kesakitan, bengkak, dan kesukaran menggerakkan kaki dengan selesa. Berita baiknya ialah banyak ketegangan tendon akan pulih dengan rehat, biasanya dalam 2 hingga 3 minggu.
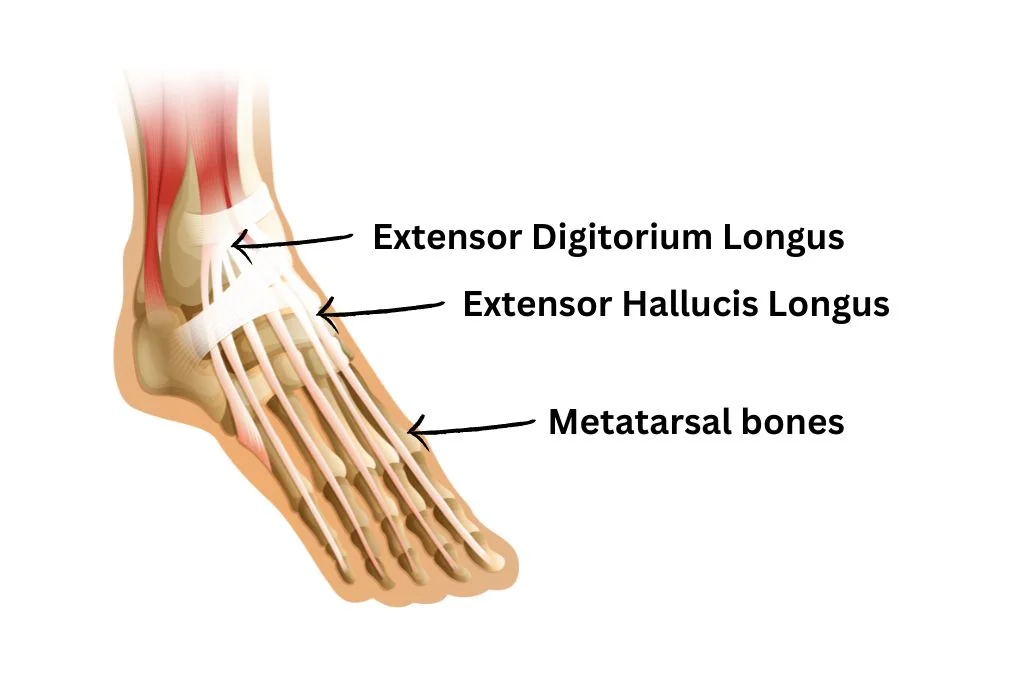
Patah Tekanan Metatarsal
Patah tulang tekanan ialah keretakan kecil pada tulang panjang kaki, biasanya disebabkan oleh tekanan berulang atau penggunaan berlebihan. Tulang metatarsal, yang terletak di kaki depan, adalah tapak biasa untuk patah tekanan. Kesakitan akibat patah tulang tekanan sering bertambah teruk dengan aktiviti dan bertambah baik dengan rehat. Anda juga mungkin melihat beberapa lebam, bengkak dan kelembutan di bahagian atas kaki.
Bursitis
Bursitis berlaku apabila bursae, kantung kecil berisi cecair yang melindungi tulang dan tendon menjadi meradang. Bursae boleh ditemui di pelbagai kawasan kaki, terutamanya di antara tendon dan tulang. Bursae di bahagian atas kaki boleh menjadi jengkel akibat geseran atau tekanan terhadap kasut atau gerakan berulang. Keradangan ini membawa kepada kesakitan, bengkak, dan kelembutan di bahagian atas kaki.
Mampatan Saraf
Mampatan saraf, atau keadaan saraf yang dikenali sebagai neuroma Morton, boleh menyebabkan kesakitan di bahagian atas kaki. Keadaan ini berpunca daripada penebalan tisu di sekeliling saraf yang membawa kepada jari kaki, menyebabkan kesakitan, sensasi terbakar, kebas dan kesemutan. Walaupun neuroma Morton biasanya menjejaskan bebola kaki, ia juga boleh menyebabkan kesakitan yang dirujuk di bahagian atas kaki. Mampatan saraf boleh disebabkan oleh kasut yang ketat atau pergerakan kaki yang tidak normal semasa aktiviti.
Artritis
Arthritis, terutamanya osteoartritis, boleh menyebabkan sakit sendi, kekakuan dan bengkak, yang boleh dirasai di bahagian atas kaki. Ia adalah hasil daripada haus dan lusuh sendi apabila seseorang semakin tua dan boleh berlaku pada mana-mana sendi kaki. Ia boleh dicetuskan oleh peningkatan mendadak dalam aktiviti dan kasut yang tidak mempunyai sokongan struktur.
Lebam dan Kecederaan
Selain kecederaan berlebihan, salah satu sebab biasa sakit kaki ialah lebam. Kesan langsung atau kecederaan pada bahagian atas kaki, seperti daripada tersandung atau jatuh, boleh menyebabkan lebam dan kesakitan serta-merta. Lebam atau kecederaan tisu lembut di bahagian atas kaki boleh mengakibatkan kesakitan, bengkak dan perubahan warna setempat.
Isu Kasut
Walaupun ini sebenarnya bukan kecederaan atau keadaan, memakai kasut atau kasut tumit tinggi yang tidak sesuai boleh menyebabkan kesakitan di bahagian atas kaki. Kasut yang terlalu ketat atau mempunyai sokongan yang tidak mencukupi boleh memampatkan bahagian atas kaki dan menyebabkan ketidakselesaan. Ini benar terutamanya untuk kasut slip-on yang mempunyai jalur elastik yang terhad di bahagian atas kaki. Oleh itu, mempelajari cara mencari kasut yang betul dengan kesesuaian yang betul adalah penting.
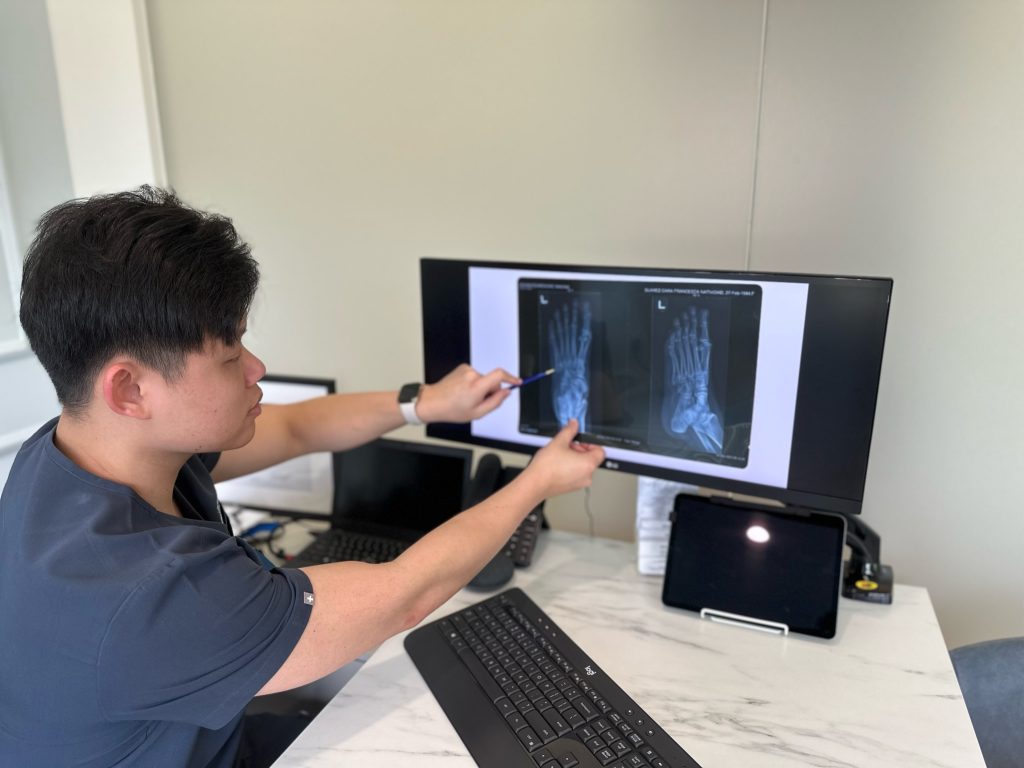
Mendiagnosis punca kesakitan di bahagian atas kaki
Diagnosis sentiasa menjadi kunci untuk mencari pengurusan yang betul. Untuk menentukan punca sakit kaki anda, kami amat mengesyorkan berunding dengan pakar kaki atau profesional perubatan. Mereka boleh melakukan penilaian menyeluruh yang terdiri daripada pemeriksaan fizikal, analisis gaya berjalan dan penilaian kasut. Penemuan mereka boleh membantu mengenal pasti punca dan menentukan sama ada penyiasatan lanjut, seperti sinar-X atau MRI, diperlukan.
Rawatan dan Pengurusan Kesakitan di Atas Kaki
Pilihan rawatan untuk kesakitan di bahagian atas kaki bergantung kepada punca asas. Pendekatan biasa yang akan kami cadangkan termasuk:
- Rehat dan Ais: Merehatkan kaki dan menggunakan ais boleh mengurangkan keradangan dan mengurangkan kesakitan.
- Footwear Adjustments: Wearing well-fitting shoes with proper support can prevent further irritation and discomfort.
- Ubat-ubatan: Ubat penahan sakit tanpa preskripsi untuk menguruskan kesakitan dan keradangan.
- Terapi Fizikal: Latihan pengukuhan dan regangan mungkin disyorkan untuk meningkatkan fungsi kaki dan mencegah masalah masa depan.
- Ortotik: Peranti ortotik tersuai boleh memberikan sokongan tambahan dan mengurangkan kesakitan yang disebabkan oleh isu struktur.
- Terapi Lanjutan: Kaedah seperti terapi gelombang kejutan boleh mempercepatkan penyembuhan semula jadi.
- Pembedahan: Dalam kes yang teruk atau apabila rawatan konservatif gagal, campur tangan pembedahan mungkin diperlukan untuk menangani isu asas.
Jangan biarkan kesakitan di atas kaki menjejaskan aktiviti anda
Sakit di bahagian atas kaki boleh disebabkan oleh pelbagai sebab, termasuk tendonitis, patah tulang tekanan, dan mampatan saraf. Mengenal pasti punca sebenar adalah penting untuk rawatan dan kelegaan yang berkesan. Jika anda sedang mengalami kesakitan yang berterusan atau teruk di bahagian atas kaki anda, dapatkan penilaian profesional lebih awal.
Di Straits Podiatry, pasukan pakar kaki kami yang berpengalaman boleh membantu memberikan anda diagnosis dan penjagaan yang sesuai. Dengan menangani punca sakit kaki anda, kami akan membantu anda kembali ke aktiviti harian anda dengan keselesaan dan fungsi yang lebih baik. Hubungi kami hari ini!
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Foot pain doesn’t just slow me down. It changes how I move, how long I can stay on my feet, and even whether I feel like doing the things I usually enjoy. However, this realisation only hits when discomfort starts affecting daily life, turning once-simple routines into cautious, calculated movements.
For those living in the East Coast of Singapore who are dealing with pain or limited mobility, it’s only natural to start searching for a podiatrist near you because travelling far for care is never feasible when every step feels like a challenge. That’s why having access to the right support in your own neighbourhood is the best approach.
Straits Podiatry’s new clinic at i12 Katong Mall offers just that. It’s a space where you can access quality care for a wide range of lower limb conditions. These include musculoskeletal and soft tissue concerns that can affect strength, stability, and overall movement. For patients with diabetes, where foot care requires added attention and coordination, our podiatrists work closely with orthopaedic specialists to manage more complex needs through a multidisciplinary approach. Whether you plan to seek relief or are looking to maintain your mobility and prevent future issues, our East Coast clinic offers the support you can count on.
Plan to Visit? Here’s What Awaits at Our East Coast Clinic
If you’re planning to visit our East Coast clinic for podiatry care, here’s what you can expect from the moment you arrive. Whether you’re seeking help with pain in your foot, skin and nail conditions, or simply want clarity on your lower limbs’ health, our team of podiatrists is here to offer care that’s transparent and thorough, all of it shaped around your actual needs, not packages or pressure.
Getting the Right Assessment Starts Here
The first step is always about listening, not rushing. When you arrive at our clinic, we begin by understanding your concerns, observing how you move, and assessing the underlying cause of your symptoms. Whether it is something long-standing or a recent issue, care begins with clarity and insight, not assumptions.
Precision Tools That Helps in the Design of Comfort
We use tools that support clinical accuracy and personalised care. These include 3D foot scanners to help us analyse structure and pressure points, as well as non-invasive modalities such as extracorporeal shockwave therapy when needed. Everything we use is selected to improve your comfort and guide the next steps of care in a focused, supportive way.
Foot Care That’s Built Around You
No two people move the same way, and no two cases are ever identical. Your care plan is shaped by your lifestyle, physical demands, and specific goals. Whether you’re trying to stay active, reduce discomfort, or manage an existing concern, we take the time to tailor an approach that fits into your everyday routine and supports long-term results.
Helping You Stay Ahead of Foot Issues
We don’t just focus on what’s already causing discomfort. A big part of our approach is helping you understand how to maintain your lower limb health and avoid future problems. This includes advice on footwear, activity levels, and small daily habits that can make a difference over time. Our goal is to help you stay informed and confident about your next steps, even after you leave the clinic.
Need Support for Any of These Foot Concerns?
More often than not, people try to coast through foot discomfort, hoping it will go away on its own. But the longer it’s ignored, the more likely it will affect how you move, how long you can stay on your feet, and how much you hold back from the things you enjoy. The cost isn’t just physical. It builds up slowly as frustration, hesitation, and the feeling that something is getting in the way. These are just some of the many conditions we review at our clinic, and if you plan to stay active and mobile, sorting them early makes all the difference. For those staying in the east, getting support is now easier with a podiatry team closer to home.
Sakit tumit
Heel pain is one of the most common reasons people seek help from podiatrists, and it often builds up slowly before it starts affecting the way you walk. For some, it shows up first thing in the morning. For others, it lingers after long hours on their feet. Whether it’s related to plantar fasciitis, achilles issues, heel spurs, or other underlying factors, early assessment helps prevent further strain and disruption.
Custom Insoles
Custom insoles are often recommended when discomfort stems from poor alignment, pressure imbalance, or structural differences in the feet. For some, discomfort builds during daily routines like walking or standing. For others, it starts to interfere with exercise or work. These insoles are prescribed by podiatrists to fit your foot shape and movement needs, helping to improve support, reduce stress, and restore balance across your lower limbs.
Kuku jari kaki yang tumbuh
Ingrown toenails can start with mild irritation but often worsen when the nail edge begins pressing into the surrounding skin and flesh. For some, discomfort stays manageable until swelling or redness appears. For others, it becomes painful enough to affect footwear choices or daily activity. Timely podiatry care can help relieve pressure, manage infection risk, and support the nail’s healthy regrowth.
Kuku kulat
Fungal nail issues often begin with subtle changes in colour, texture, or thickness. For some, it’s a cosmetic concern that gradually becomes more difficult to manage. For others, the infection causes discomfort or affects multiple toenails over time. Addressing it early can help limit the spread and support healthy regrowth before it worsens or becomes harder to control.
Ketuat Plantar
Plantar warts often appear on the parts of the foot that bear the most pressure, such as the heel or ball. What starts off looking like a rough patch can begin to feel like a pebble under the skin. As pressure builds, so does discomfort, often affecting how you stand or walk. Since these warts are viral in nature, they can also spread, which is why getting them checked early helps stop them from becoming more painful and harder to manage.
Straits Podiatry, Now Serving the East Coast
If you’ve been putting off that visit to the podiatrist or waiting for the right time to get a foot issue looked at, this is the right moment to act. With our new Straits Podiatry clinic at i12 Katong, located along 112 East Coast Road, residents in the east of Singapore now have easier access to quality foot care right in their neighbourhood.
Whether it’s a concern that has been around for a while or something more recent, our podiatrists can review your foot issues early and provide clear assessments to help you understand what’s going on. From there, we will work with you on a care plan that fits into your lifestyle and keeps things manageable over the long run.
Sometimes the cost of waiting isn’t immediately obvious. It can start with minor adjustments such as skipping walks, avoiding certain shoe models, or holding back from the things you usually enjoy doing. When these become part of your routine, it might be time to speak with someone who can help. Contact us today to book an appointment or have a quick word with our podiatrists. Taking that step earlier can make it easier to stay on top of discomfort and prevent bigger issues from setting in.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Jangkitan kaki kulat, seperti kulat kaki atlet dan kuku kaki, adalah keadaan biasa yang menjejaskan ramai individu. Walaupun berleluasa, jangkitan ini boleh menjadi sukar untuk dirawat dan degil untuk disingkirkan. Memahami mengapa jangkitan kulat pada kaki sukar diuruskan boleh membantu mendapatkan rawatan yang berkesan dan mencegah kejadian pada masa hadapan.
Apakah Jangkitan Kaki Kulat?
Jangkitan kaki kulat disebabkan oleh pelbagai jenis kulat yang tumbuh subur dalam persekitaran yang hangat dan lembap. Di Singapura, iklim kita menjadikannya sesuai untuk kulat tumbuh dan membiak. Oleh itu, jangkitan kaki kulat adalah salah satu jangkitan kulit yang paling biasa di sini.
Jangkitan kulat kaki yang paling biasa termasuk:
- Kaki Atlet (Tinea Pedis): Menjejaskan kulit antara jari kaki dan tapak kaki, menyebabkan gatal-gatal, kemerahan dan mengelupas.
- Kulat kuku kaki (Onychomycosis): Memberi kesan kepada kuku kaki, membawa kepada kuku yang menebal, berubah warna dan rapuh.

Faktor-faktor yang menyumbang kepada kesukaran merawat jangkitan kulat
1. Daya Tahan dan Kegigihan Kulat
Kulat ialah organisma berdaya tahan yang mampu bertahan dalam pelbagai persekitaran. Mereka boleh berterusan pada permukaan, dalam kasut, dan juga pada kulit. Daya tahan ini menjadikannya mencabar untuk menyingkirkan jangkitan sepenuhnya, kerana kulat boleh kekal tidak aktif dan menjangkiti semula kawasan tersebut jika tidak dirawat dengan teliti.
2. Kerumitan Rawatan Jangkitan Kulat
Oleh kerana daya tahan mereka, rawatan jangkitan kaki kulat sering memerlukan pendekatan pelbagai rupa. Ini boleh termasuk ubat oral, aplikasi topikal, atau terapi antikulat PACT. Ubat antikulat, sama ada topikal atau oral, mesti terlebih dahulu dapat menembusi atau mencapai kawasan yang dijangkiti dengan berkesan. Penembusan adalah salah satu faktor utama dalam rawatan kulat kuku, kerana jangkitan ocmenyembuhkan di bawah kuku kaki. Ia juga penting untuk melengkapkan kursus rawatan untuk menghapuskan dan mengurangkan risiko jangkitan semula.
3. Kesukaran dalam Diagnosis
Diagnosis yang tepat adalah penting untuk rawatan yang berkesan. Jangkitan kulat boleh meniru keadaan lain seperti psoriasis atau ekzema. Salah diagnosis boleh membawa kepada rawatan yang tidak sesuai, memanjangkan jangkitan dan menjadikannya lebih sukar untuk ditangani. Contoh yang paling biasa ialah menggunakan krim steroid untuk jangkitan kaki kulat, yang pada asasnya akan memburukkan keadaan dari semasa ke semasa. Oleh itu, jika anda ragu-ragu, sentiasa dapatkan pendapat daripada pakar kaki atau pakar dermatologi.
4. Rintangan Kulat
Sesetengah kulat telah mengembangkan ketahanan terhadap ubat antikulat biasa, menjadikannya lebih sukar untuk dirawat. Rintangan ini boleh disebabkan oleh kursus rawatan yang tidak lengkap atau penggunaan produk antikulat yang berlebihan, yang boleh menggalakkan perkembangan strain kulat tahan. Oleh itu, kami amat mengesyorkan hanya menggunakan produk di bawah pengawasan atau nasihat profesional.
5. Risiko Jangkitan Semula
Jangkitan kaki kulat boleh menjadi agak berjangkit dan mudah merebak di kawasan komunal seperti gimnasium, kolam renang dan bilik persalinan. Amalan kebersihan yang tidak mencukupi, berkongsi barangan peribadi, atau berjalan tanpa alas kaki di tempat awam boleh menyebabkan jangkitan semula atau penularan kepada orang lain.
6. Sifat Kronik Beberapa Jangkitan
Jangkitan kulat tertentu, terutamanya kulat kuku kaki, adalah kronik dan memerlukan rawatan yang berpanjangan untuk memastikan pembasmian sepenuhnya. Kadar pertumbuhan kuku kaki yang perlahan bermakna ia boleh mengambil masa beberapa bulan untuk melihat peningkatan yang ketara, dan rawatan yang tidak lengkap boleh mengakibatkan berulang.

Strategi untuk Pengurusan dan Pencegahan yang Berkesan
1. Dapatkan Bantuan Profesional Lebih Awal
Pengesanan dan pengurusan awal membantu dalam mencegah penyebaran selanjutnya dan meningkatkan kadar kejayaan. Mempunyai penilaian profesional juga memastikan bahawa ubat antikulat yang betul digunakan dan keadaan lain diketepikan.
2. Patuhi Protokol Rawatan
Lengkapkan kursus penuh ubat antikulat yang ditetapkan, walaupun gejala bertambah baik sebelum menamatkan rawatan. Ini membantu mencegah jangkitan berulang dan mengurangkan risiko mengembangkan strain kulat tahan.
3. Amalkan Kebersihan Kaki yang Baik
Kekalkan kebersihan kaki yang baik dengan memastikan kaki bersih dan kering. Tukar stokin dan kasut dengan kerap, dan elakkan berjalan tanpa alas kaki di kawasan awam. Gunakan serbuk atau semburan antikulat sebagai langkah pencegahan dalam persekitaran komunal. Elakkan berkongsi stokin atau kasut dengan orang lain.
4. Membasmi kuman barangan peribadi
Nyahkuman kasut, stokin dan barangan peribadi lain yang mungkin bersentuhan dengan kawasan yang dijangkiti. Ini membantu menghapuskan spora kulat dan mengurangkan risiko jangkitan semula. Anda boleh berbuat demikian dengan pembasmi kuman di kaunter atau mencucinya dengan air panas.
Pantau dan Uruskan Faktor Risiko
Tangani sebarang keadaan asas yang boleh menyumbang kepada jangkitan kulat, seperti kulit kering, diabetes atau masalah sistem imun. Menguruskan keadaan ini boleh membantu mengurangkan risiko jangkitan berulang.
Kesimpulan
Jangkitan kulat pada kaki boleh mencabar untuk dirawat disebabkan oleh faktor-faktor seperti daya tahan kulat, kerumitan rawatan, kesukaran dalam diagnosis, dan risiko jangkitan semula. Walau bagaimanapun, dengan penjagaan perubatan yang sesuai, pematuhan kepada protokol rawatan, dan langkah pencegahan, adalah mungkin untuk mengurus dan mengatasi jangkitan ini dengan berkesan.
Jika anda mengesyaki jangkitan kaki kulat, dapatkan penilaian profesional daripada pakar kaki kami di Straits Podiatry hari ini!
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Ingrown toenails can be a painful and recurring issue for many individuals. It often requires early effective treatment to alleviate discomfort and prevent further complications. One innovative ingrown toenail treatment approach gaining attention recently is nail bracing or nail braces.
But does it really work? Let’s find out what nail braces are and their effectiveness in managing ingrown toenails!
Memahami kuku jari kaki yang tumbuh
Kuku jari kaki yang tumbuh berlaku apabila tepi kuku tumbuh ke kulit di sekeliling katil kuku, yang membawa kepada kesakitan, bengkak, dan jangkitan yang berpotensi. Sebab-sebab biasa termasuk pemangkasan kuku yang tidak betul, trauma, atau struktur kuku yang diwarisi.
What is a Nail Brace?
Nail bracing is a noninvasive ingrown toenail treatment method that corrects the nail shape without the need for surgery. It involves applying a thin strip made of compound polymer to the affected nail. This device exerts gentle pressure to gradually lift the nail’s edge away from the skin. This reduces the tendency for the nail to grow into the surrounding tissue.
Bagaimana Bracing Kuku Berfungsi?
The principle behind nail bracing is to reshape the nail over time, encouraging it to grow outwards rather than into the skin. The nail braces are carefully applied by a trained podiatrist and are comfortable and discreet. They work by:
- Mengangkat Kuku: Dengan mengangkat tepi kuku yang tumbuh, pendakap membantu melegakan tekanan pada kulit di sekelilingnya, mengurangkan kesakitan dan keradangan.
- Menggalakkan Pertumbuhan yang Betul: Apabila kuku tumbuh, pendakap membimbingnya untuk berkembang ke arah yang lebih lurus dan lebih sihat, meminimumkan risiko berulang.

Keberkesanan Bracing Kuku
Penyelidikan dan pengalaman klinikal menunjukkan bahawa bracing kuku boleh menjadi pilihan rawatan yang berkesan, terutamanya untuk kes-kes ringan kuku jari kaki. Faedah termasuk:
- Tidak invasif: Tidak seperti kaedah pembedahan tradisional, bracing kuku tidak invasif dan tidak memerlukan pemotongan atau penyingkiran kuku yang terjejas.
- Ketidakselesaan Minimum: Pesakit biasanya melaporkan ketidakselesaan minimum semasa dan selepas penggunaan pendakap.
- Kadar Kejayaan yang Menjanjikan: Apabila digunakan dengan betul dan bersama-sama dengan teknik penjagaan kuku yang betul, bracing kuku telah menunjukkan hasil yang baik dalam membetulkan kuku jari kaki yang tumbuh dan mencegah pengulangannya.
Adakah Bracing Kuku Sesuai untuk Anda?
Bracing kuku adalah paling sesuai untuk individu yang mempunyai kuku jari kaki ringan hingga sederhana yang lebih suka pendekatan bukan pembedahan atau ingin mengelakkan tempoh pemulihan yang berkaitan dengan pembedahan kuku jari kaki yang tumbuh. Walau bagaimanapun, ia mungkin tidak sesuai untuk kes-kes yang teruk atau mereka yang mempunyai keadaan kesihatan asas yang mempengaruhi kaki. Ia juga mungkin tidak berfungsi dengan baik dalam kes-kes yang rumit oleh kulat kuku.
Cara Bermula
Sekiranya anda mengalami ketidakselesaan dari kuku jari kaki yang tumbuh dan sedang mempertimbangkan bracing kuku sebagai pilihan rawatan, adalah penting untuk berunding dengan podiatrist yang berkelayakan. Semasa perundingan anda, podiatrist harus menilai keadaan anda, membincangkan matlamat rawatan anda, dan menentukan sama ada rawatan itu sesuai untuk anda.
Kesimpulan
Bracing kuku menawarkan alternatif yang menjanjikan untuk campur tangan pembedahan untuk merawat kuku jari kaki yang tumbuh, menyediakan penyelesaian yang tidak invasif dengan hasil jangka panjang. Dengan menangani corak pertumbuhan kuku yang mendasari, bracing kuku boleh membantu mengurangkan kesakitan, mengurangkan keradangan, dan mencegah kejadian kuku jari kaki yang tumbuh di masa depan.
Jika anda mencari bantuan daripada kuku jari kaki yang menyakitkan, pertimbangkan bracing kuku sebagai pilihan. Rujuk Podiatrist kami untuk mendapatkan nasihat hari ini!
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Tendon Achilles koyak atau pecah boleh menjadi kecederaan yang melemahkan, sering menjejaskan atlet dan individu aktif. Memahami tanda-tanda dan gejala boleh membantu anda mengenal pasti jika anda mungkin dari keadaan ini. Berikut ialah panduan komprehensif untuk mengiktiraf air mata tendon Achilles:
Memahami Tendon Achilles
Tendon Achilles adalah tendon terbesar dalam badan, menghubungkan otot betis ke tulang tumit. Ia memainkan peranan penting dalam berjalan, berlari, dan melompat. Apabila tendon ini terlalu banyak atau koyak, ia boleh menyebabkan kesakitan yang ketara dan mobiliti terjejas. Air mata tendon Achilles berbeza daripada tendinitis Achilles, yang merupakan keradangan tendon tanpa air mata.
Punca yang paling biasa koyak tendon Achilles atau pecah adalah sukan. Ini terutama berlaku untuk sukan yang memerlukan pergerakan seperti lunges atau lompatan. Contoh aktiviti tersebut ialah badminton, tenis, atau bola keranjang.
Tanda dan Gejala Air Mata Tendon Achilles
- Kesakitan yang tiba-tiba dan teruk: Salah satu gejala tanda air mata tendon Achilles adalah kesakitan yang tiba-tiba dan tajam di belakang buku lali atau anak lembu. Ini sering berlaku semasa aktiviti fizikal atau pergerakan secara tiba-tiba.
- Bengkak dan Kelembutan: Berikutan kecederaan, anda mungkin melihat bengkak di sekitar tumit dan buku lali. Kawasan ini juga mungkin berasa lembut untuk disentuh, menunjukkan keradangan dan kerosakan pada tendon.
- Kesukaran Berjalan atau Berdiri di Atas Jari Kaki: Air mata tendon Achilles boleh menjadikannya mencabar untuk berdiri di hujung kaki atau menolak kaki yang terjejas semasa berjalan. Ini disebabkan oleh ketidakupayaan tendon yang lemah atau rosak untuk menyokong pergerakan ini.
- Sensasi "Pop": Sesetengah individu melaporkan pendengaran atau merasakan "pop" pada masa kecederaan. Sensasi ini sering mengiringi air mata tendon Achilles dan diikuti dengan kesakitan dan kelemahan segera di kaki.
- Lebam: Dalam kes-kes yang teruk, lebam boleh berkembang di sekitar kawasan tumit dan buku lali. Ini berlaku kerana pendarahan dalam tisu sekitar tendon koyak.
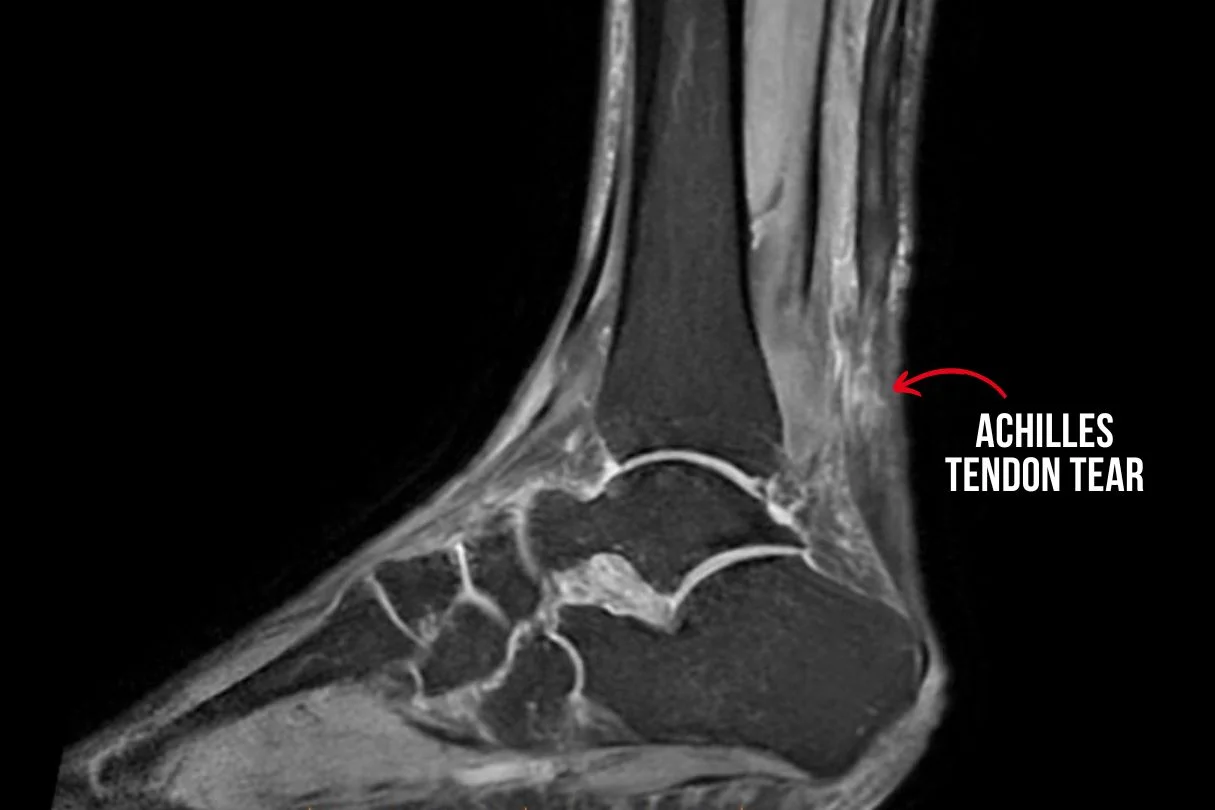
Diagnosis dan Rawatan
Jika anda mengalami gejala-gejala ini dan mengesyaki bahawa anda mungkin mengalami koyakan tendon Achilles, adalah penting untuk mendapatkan rawatan perubatan dengan segera. Pakar podiatrist atau ortopedik boleh melakukan pemeriksaan fizikal, memeriksa tanda-tanda yang relevan dan menilai struktur tendon Achilles.
Ujian diagnostik seperti ultrasound atau imbasan MRI biasanya diperlukan untuk mengesahkan tahap kecederaan. Pilihan rawatan bergantung kepada keterukan air mata tetapi biasanya termasuk:
- Rehat dan Imobilisasi: Menjaga berat badan dari kaki yang cedera dan menggunakan tongkat atau but berjalan untuk membolehkan tendon sembuh.
- Senaman dan Pengukuhan: Latihan pemulihan secara beransur-ansur untuk menguatkan otot betis dan meningkatkan fleksibiliti.
- Terapi Lanjutan: Terapi regeneratif, seperti terapi gelombang kejutan atau terapi medan elektromagnet berdenyut, boleh merangsang penyembuhan semula jadi tendon.
- Pembaikan Pembedahan: Dalam kes koyakan lengkap atau kecederaan teruk, pembedahan mungkin diperlukan untuk memasang semula hujung tendon dan memulihkan fungsi.

Pemulihan dan Pencegahan
Pulih dari air mata tendon Achilles boleh menjadi proses yang panjang, selalunya memerlukan beberapa bulan pemulihan. Walau bagaimanapun, dengan penjagaan yang betul dan pematuhan kepada protokol rawatan, ramai individu boleh mendapatkan semula fungsi penuh pergelangan kaki mereka dan kembali ke tahap aktiviti sebelumnya.
Untuk mengelakkan kecederaan tendon Achilles, adalah penting untuk:
- Memanaskan dan Regangan: Sebelum melakukan aktiviti fizikal, pastikan otot anda dipanaskan dan diregangkan dengan secukupnya.
- Secara beransur-ansur meningkatkan intensiti: Elakkan peningkatan mendadak dalam intensiti atau tempoh latihan, yang boleh menimbulkan tendon Achilles.
- Gunakan Kasut Sokongan yang Betul: Pakai kasut sokongan yang sesuai untuk aktiviti anda, terutamanya jika anda mengambil bahagian dalam sukan yang melibatkan berlari atau melompat.
Dengan mengenali tanda-tanda tendon Achilles koyak lebih awal dan mendapatkan rawatan tepat pada masanya, anda boleh meningkatkan hasil dan meminimumkan risiko komplikasi jangka panjang. Jika anda mengesyaki anda mungkin mengalami kecederaan tendon Achilles anda, jangan teragak-agak untuk berunding dengan profesional penjagaan kesihatan untuk penilaian menyeluruh dan pelan rawatan peribadi.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Pengenalan
Pergelangan kaki adalah struktur rumit yang membolehkan kita berdiri, berjalan, dan bergerak. Memahami anatomi pergelangan kaki adalah penting dalam diagnosis atau pengurusan sebarang keadaan buku lali. Tanpa pengetahuan tentang bagaimana sendi pergelangan kaki dibuat, mustahil bagi mana-mana profesional perubatan untuk mengenal pasti struktur mana yang cedera atau meradang. Oleh itu dalam artikel ini, kita akan membongkar fakta asas mengenai struktur yang membentuk sendi buku lali.
Anatomi pergelangan kaki: strukturnya
Sendi buku lali anda adalah keajaiban kejuruteraan, yang terdiri daripada beberapa komponen penting yang bekerjasama untuk menyokong pergerakan anda. Berikut adalah pecahan perkara yang membentuk buku lali anda:
Tulang
Bayangkan buku lali anda sebagai jambatan antara kaki dan kaki anda. Tulang utama yang terlibat ialah tibia (tulang shinbone), fibula (tulang betis), dan talus (tulang buku lali). Bersama-sama, mereka membentuk struktur kukuh yang membolehkan anda berjalan, berlari, dan melompat dengan mudah. Mereka adalah asas anatomi pergelangan kaki.
Ligamen
Gambar tali kecil yang memegang sendi buku lali anda bersama-sama. Ini adalah ligamen, dan mereka memainkan peranan penting dalam memastikan buku lali anda stabil. Ia menghalang buku lali anda daripada bergolek terlalu jauh ke dalam atau ke luar, mengurangkan risiko terseliuh.
5 ligamen penting di bahagian medial (dalam), yang dikenali sebagai ligamen deltoid pergelangan kaki adalah:
- Ligamen tibiocalcaneal - menghubungkan tulang tibia ke tulang tumit
- Ligamen Talonavicular - menghubungkan tulang talus ke tulang navicular
- Anterior tibiotalar – menghubungkan tulang tibia ke tulang talus di bahagian hadapan buku lali
- Tibiotalar posterior yang cetek dan mendalam - kedua-duanya menghubungkan tulang tibia ke tulang talus di bahagian belakang buku lali
Terdapat 3 ligamen utama di bahagian sisi (luar) pergelangan kaki:
- Ligamen talofibular anterior - menghubungkan tulang fibula ke tulang talus di bahagian depan buku lali
- Ligamen talofibular posterior - menghubungkan tulang fibula ke tulang talus di bahagian belakang buku lali
- Ligamen calcaneofibular - menghubungkan tulang fibula ke tulang tumit
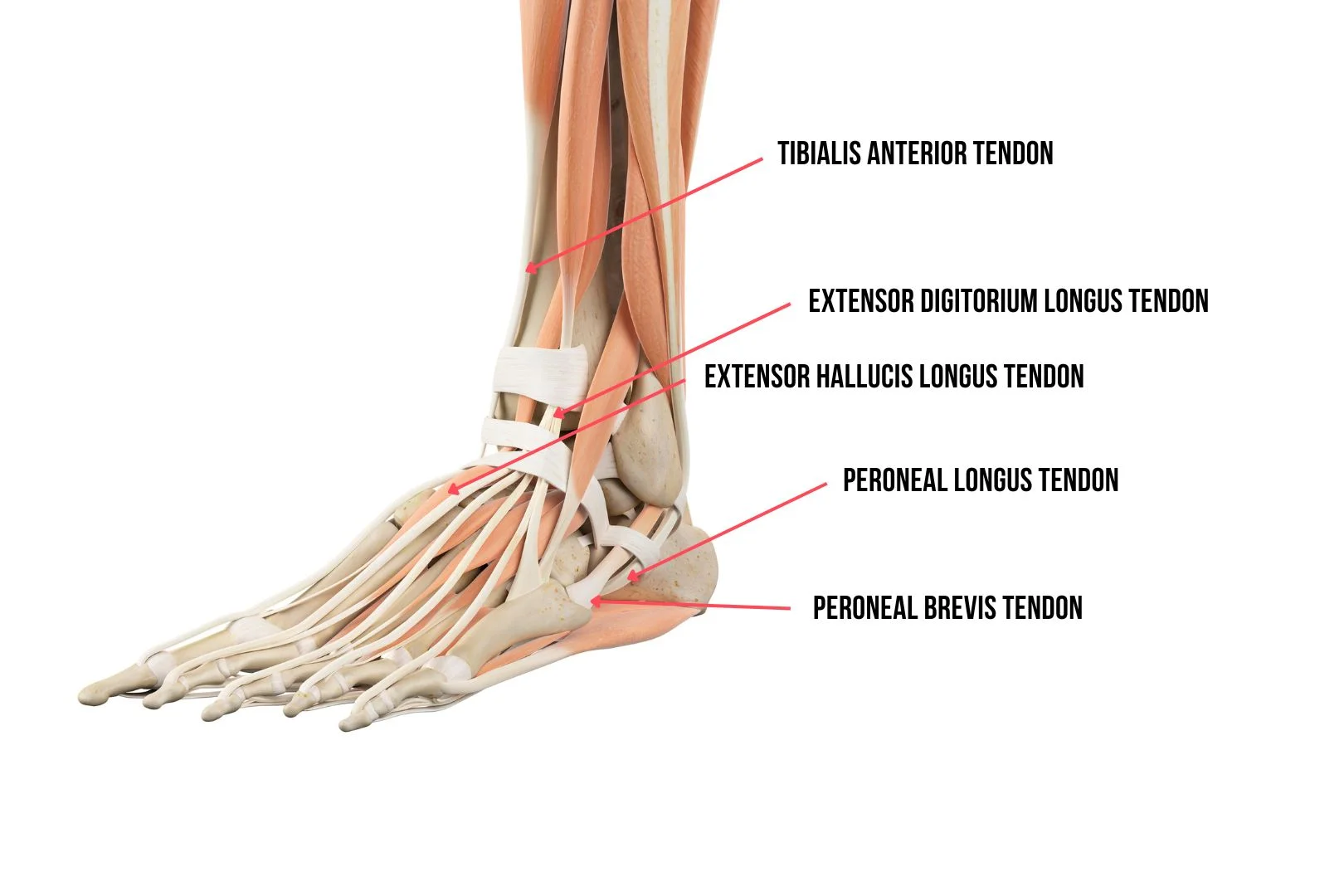
Tendon
Tendon adalah seperti gelang getah kuat yang menghubungkan otot ke tulang. Tendon Achilles adalah yang terbesar di seluruh anatomi pergelangan kaki dan menghubungkan otot betis ke tulang tumit. Ia membantu anda menolak tanah apabila anda berjalan atau berlari. Tendon penting lain yang terdapat di sekitar pergelangan kaki adalah:
- Tibialis anterior tendon
- Tibialis posterior tendon
- Extensor Hallucis longus tendon
- Extensor digitorium longus tendon
- Tendon Longus Peroneus
- Peroneus brevis tendon
- Flexor hallucis longus tendon
- Flexor digitorium longus tendon
Otot
Buku lali anda dikuasakan oleh rangkaian otot yang berfungsi bersama-sama untuk menggerakkan kaki anda ke atas dan ke bawah. Otot betis, termasuk gastrocnemius dan soleus, membantu anda menunjuk jari kaki anda ke bawah (plantarflexion), manakala otot di bahagian depan kaki anda, seperti anterior tibialis, membantu anda mengangkat jari kaki anda (dorsiflexion). Setiap tendon di atas disambungkan ke otot masing-masing, dan bersama-sama, mereka bekerja bersama-sama untuk mengawal pergerakan kaki dan buku lali anda.
Mengapa Anatomi Buku Lali Penting
Memahami asas anatomi buku lali adalah penting untuk semua orang, bukan hanya atlet atau profesional penjagaan kesihatan. Dengan mengetahui bagaimana pergelangan kaki anda berstruktur dan bagaimana ia berfungsi, anda boleh:
- Jaga buku lali anda dengan lebih baik dengan mengelakkan aktiviti yang boleh membebankan mereka.
- Kenali tanda-tanda kecederaan, seperti terseliuh buku lali atau patah tulang, dan dapatkan rawatan kecederaan buku lali dengan segera.
- Kenali tanda-tanda awal kecederaan tendon berdasarkan lokasi kesakitan, seperti tendonitis tibial posterior, tendonitis Achilles, atau tendonitis peroneal
- Sokong kesihatan buku lali anda melalui senaman dan regangan yang menguatkan otot sekitarnya.
Kesimpulan
Seperti yang telah anda pelajari, pergelangan kaki anda adalah struktur yang luar biasa yang membolehkan anda bergerak dengan rahmat dan kemudahan. Dengan mendapatkan gambaran tentang anatomi buku lali dan fungsi, anda boleh menghargai kepentingan menjaga mereka dengan betul. Sama ada anda berjalan, menari, atau hanya berdiri, pergelangan kaki anda sukar di tempat kerja, menyokong anda setiap langkah. Oleh itu, luangkan sedikit masa untuk mengucapkan terima kasih kepada buku lali anda untuk semua yang mereka lakukan, dan ingatlah untuk merawat mereka dengan kebaikan dan penjagaan yang mereka layak.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Kaki rata, atau gerbang jatuh, boleh menyebabkan ketidakselesaan dan kesakitan bagi ramai individu, memberi kesan kepada aktiviti harian dan kualiti hidup mereka. Nasib baik, pasangan insole yang betul boleh memberikan kelegaan dan sokongan yang ketara. Dalam artikel ini, kami akan menerangkan petunjuk, fungsi, dan faedah insole untuk kaki rata di Singapura.
Memahami Kaki Rata
Kaki rata, atau Pes Planus, berlaku apabila gerbang kaki runtuh, menyebabkan seluruh tapak untuk menghubungi tanah. Keadaan ini boleh menjadi genetik (diturunkan dari ibu bapa) atau berkembang dari masa ke masa akibat kecederaan, penuaan, atau kedudukan yang berpanjangan. Disfungsi tendon tibial posterior adalah salah satu kecederaan kaki yang paling biasa yang menyebabkan gerbang runtuh dari masa ke masa. Individu yang mempunyai kaki rata sering mengalami gejala seperti sakit kaki, bengkak, dan kesukaran berdiri atau berjalan untuk tempoh yang lama.
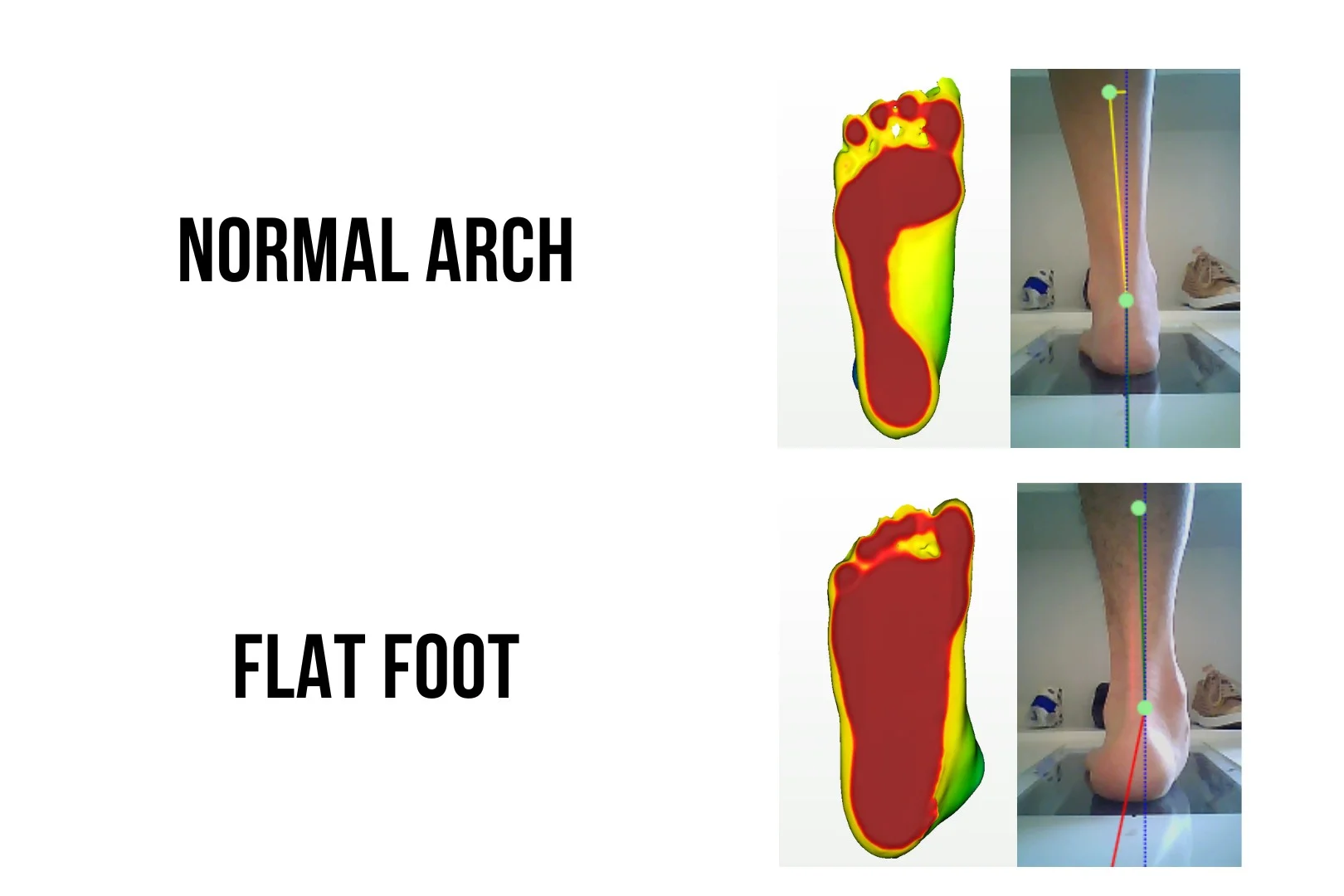
Bagaimanakah Insoles boleh membantu kaki rata?
Insoles, juga dikenali sebagai ortotik kaki, adalah sisipan kasut yang direka khas yang sesuai dengan kasut untuk memberikan sokongan, kestabilan, dan kusyen untuk kaki. Insole generik boleh didapati secara meluas di pasaran dan biasanya sesuai untuk individu yang mempunyai kaki biasa dan isu-isu minimum. Walau bagaimanapun, bagi individu yang mempunyai kaki rata, insole tersuai biasanya disyorkan untuk membantu menyusun semula postur kaki.
Sepasang insole kaki rata yang ideal harus mengurangkan pronasi yang berlebihan, di mana pergelangan kaki bergolek ke dalam semasa berdiri dan berjalan. Dengan mengurangkan pronasi yang berlebihan, insole kaki rata akan mengurangkan tekanan pada otot, sendi dan ligamen kaki. Ini juga boleh menyebabkan tindak balas rantai sehingga kaki dan belakang bawah, mengurangkan tekanan pada lutut, pinggul, dan punggung bawah kita. Insole kaki rata dengan reka bentuk yang betul pasti dapat meningkatkan fungsi kaki secara keseluruhan dan mengurangkan sakit lutut dan sakit belakang bawah.
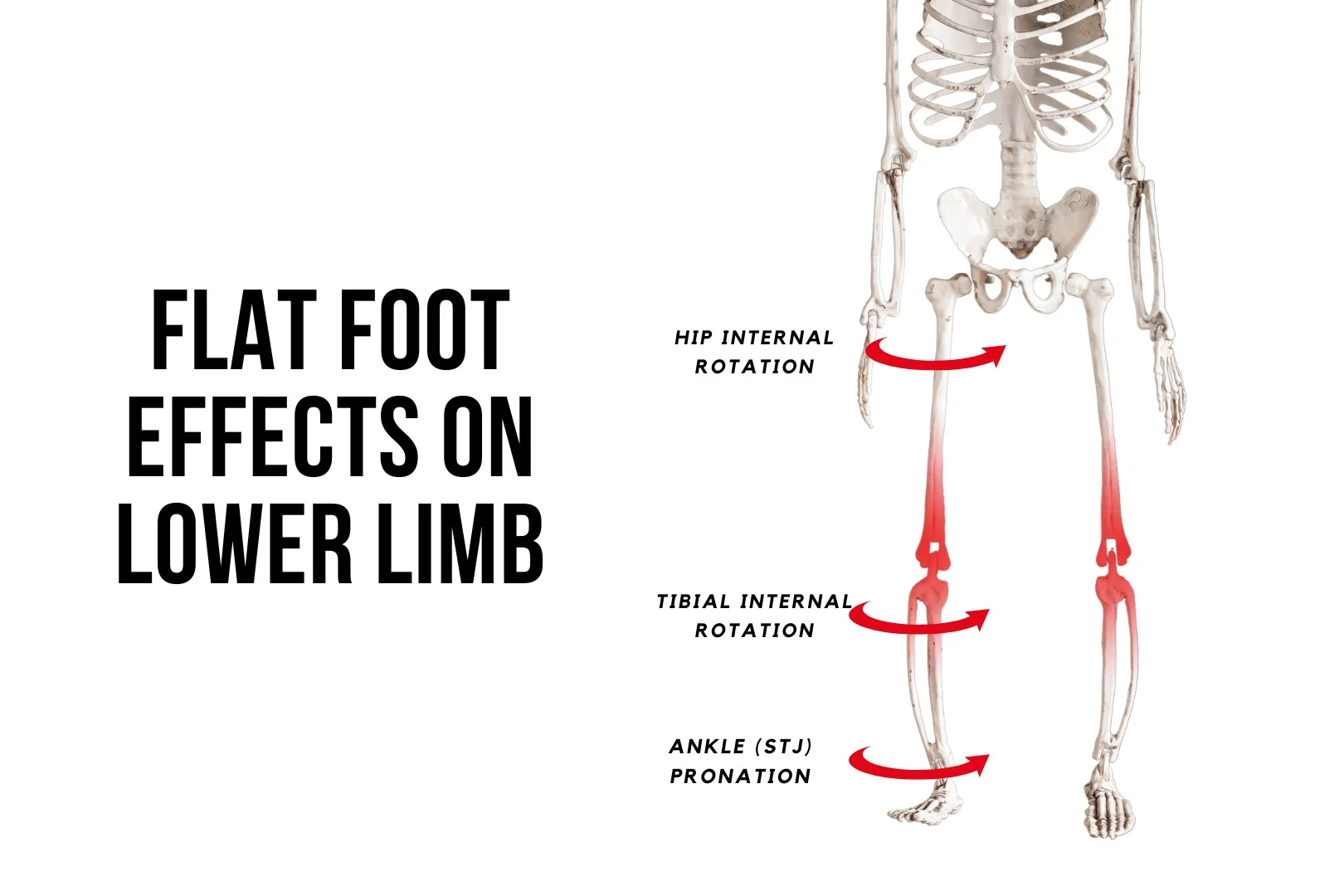
Bagaimanakah Insoles Kaki Rata Berfungsi?
Salah faham yang paling biasa tentang insoles untuk kaki rata ialah mereka memberikan sokongan gerbang. Walau bagaimanapun, sokongan gerbang tidak selesa bagi kebanyakan individu dengan kaki rata yang ketara. Ia biasanya menyebabkan kesakitan dan ketidakselesaan di sepanjang lengkungan, dan kebanyakan orang tidak boleh bertolak ansur. Ini kerana sokongan lengkungan sahaja hanya memberi tekanan kepada lengkungan dan tidak mengubah postur kaki.
Insoles kaki rata, apabila dibuat dengan betul, biasanya akan menyebabkan perubahan postur kaki. Satu-satunya pengecualian ialah apabila seseorang mempunyai kecacatan kaki yang tegar. Insoles harus mempunyai ciri-ciri yang cekap menggunakan daya di lokasi kanan kaki dan condongkan kaki ke luar. Perubahan postur kaki akan mengurangkan tekanan yang bertindak pada tendon, ligamen, dan sendi dan memberikan kelegaan kepada individu.
Sepasang insole kaki rata yang direka dengan baik harus menggabungkan ciri-ciri berikut:
- Jumlah kecondongan tumit yang ideal (varus kaki belakang)
- Lokasi puncak gerbang yang diletakkan dengan betul
- Cawan tumit dalam untuk menyokong tumit
- Pengubahsuaian untuk menggunakan daya supinasi untuk menyusun semula kaki
- Keseimbangan daya dan perubahan sudut yang baik bertindak pada kaki (kinetik vs kinematik)
Setiap sepasang insoles adalah unik kerana keterukan kaki rata berbeza antara individu.
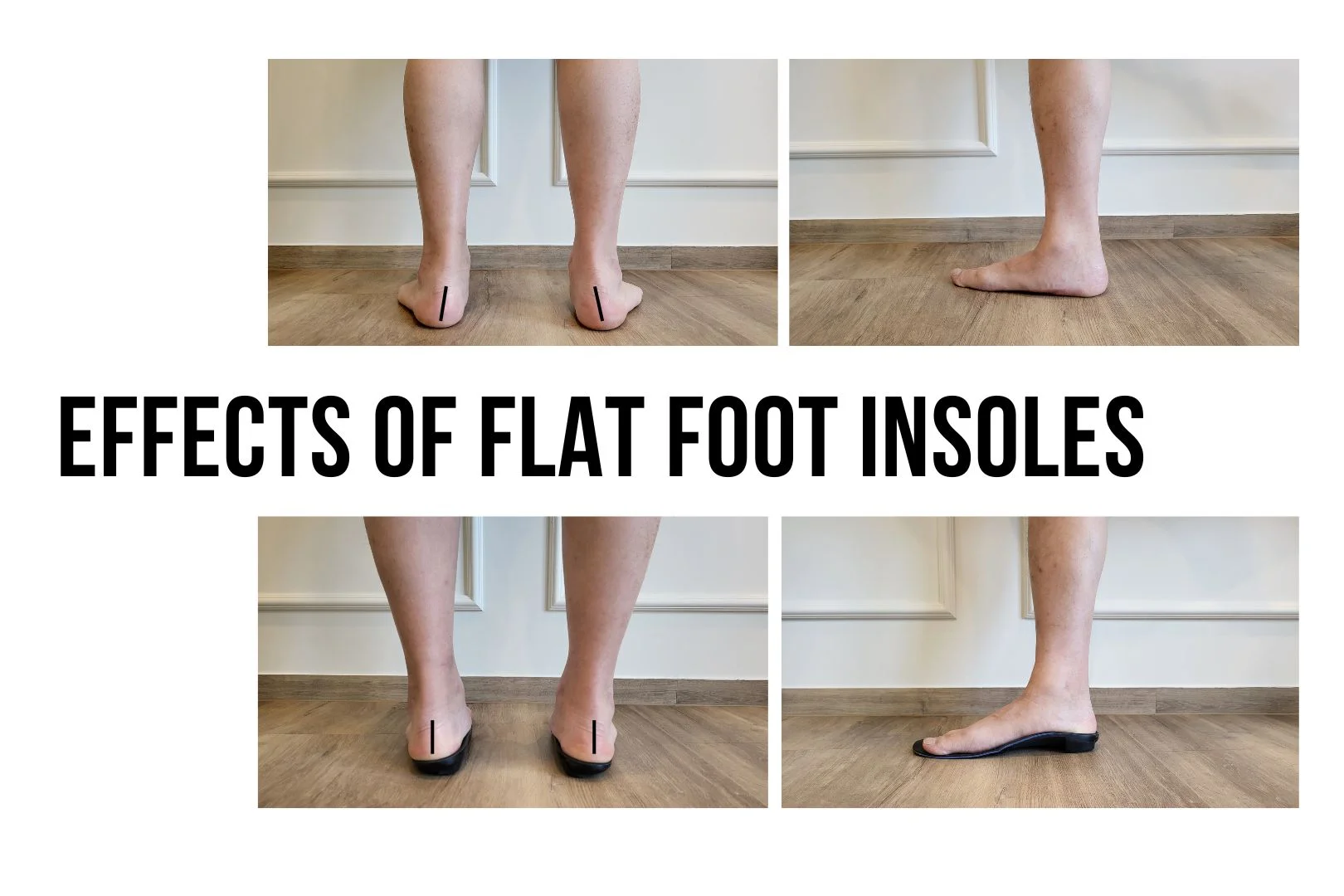
Insoles Kaki Rata Tersuai di Straits Podiatry
Di Straits Podiatry, kami memahami bagaimana mencari insole yang sesuai untuk kaki rata adalah penting untuk mengekalkan kesihatan kaki dan mobiliti. Sepasang insole berkualiti tinggi boleh membuat perbezaan yang signifikan dalam mengurangkan kesakitan dan ketidakselesaan, membolehkan anda kekal aktif dan mudah alih. Pasukan podiatrik kami yang berkelayakan mempunyai pengalaman peribadi dengan kaki rata dan boleh membantu anda menguruskan keadaan anda. Sekiranya anda ingin mengetahui lebih lanjut mengenai insoles untuk kaki rata, sila hubungi kami atau buat temujanji hari ini!
Soalan lazim
Adakah insole kaki rata tidak selesa dipakai?
Apabila reka bentuk itu sesuai, insole kaki rata tersuai tidak boleh menyebabkan ketidakselesaan. Ketidakselesaan biasanya timbul apabila insoles mengenakan terlalu banyak tekanan pada lengkungan tanpa perubahan postur kaki. Walau bagaimanapun, anda mungkin memerlukan beberapa minggu untuk menyesuaikan diri dengan perubahan corak berjalan pada mulanya.
Berapa lama insoles bertahan?
Bergantung pada bahan yang digunakan, sepasang insole kaki rata tersuai boleh bertahan antara 1 hingga 3 tahun. Faktor-faktor yang boleh mempercepatkan haus dan lusuh adalah jumlah aktiviti fizikal yang anda lakukan, dari segi kekerapan dan intensiti. Insoles untuk orang dewasa yang bekerja biasa biasanya bertahan lebih lama daripada pelari maraton.
Bolehkah insole kaki rata digunakan dalam kasut yang berbeza?
Ya awak boleh. Walau bagaimanapun, ini tidak terpakai kepada semua jenis kasut. Nasihat umum kami ialah insole kaki rata biasanya boleh memuatkan kebanyakan kasut sukan dan kasut. Mungkin terdapat batasan apabila cuba menyesuaikannya dengan kasut kulit atau kasut mahkamah wanita, dan dalam kes sedemikian, reka bentuk yang berbeza boleh dibuat agar sesuai dengan kasut ini.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Di Straits Podiatry, kita faham bagaimana trauma kuku yang menyedihkan. Sama ada ia timbul daripada seseorang yang memijak kaki anda atau mengetuk pintu, ia boleh menjadi sangat menyakitkan dan menjejaskan aktiviti harian anda. Dalam artikel ini, kami akan membincangkan sebab, gejala, dan pilihan rawatan trauma kuku untuk membantu anda memahami cara mencegah dan menguruskan kecederaan ini.
Punca Trauma Kuku:
Trauma kuku boleh disebabkan oleh pelbagai sebab, termasuk:
- Kemalangan: Stubbing jari kaki anda atau menjatuhkan objek berat di kaki anda.
- Aktiviti sukan: Sukan yang melibatkan berlari atau melompat, seperti bola keranjang atau bola sepak, terutamanya jika kasut anda terlalu ketat atau tidak sesuai dengan betul.
- Kasut yang tidak betul: Memakai kasut yang terlalu ketat atau longgar boleh menyebabkan geseran dan tekanan pada kuku jari kaki anda, yang membawa kepada trauma.
- Jangkitan kulat: Jangkitan kuku kulat boleh menyebabkan kuku menjadi lebih tebal dan melengkung, menjadikannya lebih mudah terdedah kepada trauma.
Gejala Trauma Kuku:
Gejala trauma kuku bergantung pada tahap kecederaan, tetapi tanda-tanda biasa termasuk:
- Perubahan warna: Lebam atau lepuh darah di bawah kuku boleh menyebabkan kuku menjadi hitam, biru, atau ungu.
- Kesakitan: Trauma kuku boleh menyakitkan, terutamanya apabila berjalan atau di bawah tekanan
- Bengkak: Bengkak di sekeliling kuku boleh berlaku, menjadikannya sukar untuk memakai kasut.
- Perubahan dalam bentuk kuku: Sekiranya terdapat kerosakan pada katil kuku, kuku boleh tumbuh kembali lebih tebal atau mengembangkan rabung atau benjolan. Ia juga boleh membawa kepada keadaan kuku jari kaki yang menyakitkan .
- Lepuh darah di bawah kuku: Hematoma subungual boleh terbentuk di bawah kuku, biasanya akibat pendarahan dari katil kuku.

Rawatan untuk Trauma Kuku:
Pelbagai pilihan rawatan trauma kuku termasuk:
- Rehat dan Ketinggian: Berehat dan mengangkat kaki yang terjejas dapat mengurangkan bengkak dan kesakitan.
- Ais: Memohon ais ke kawasan yang cedera juga boleh membantu mengurangkan bengkak dan kesakitan.
- Antibiotik: Sekiranya terdapat jangkitan, kami mungkin menetapkan antibiotik untuk membantu membersihkan jangkitan.
- Penyingkiran Kuku: Dalam kes-kes yang teruk di mana kuku rosak teruk atau dijangkiti, avulsion kuku mungkin diperlukan.
- Pembedahan: Dalam kes-kes yang jarang berlaku, pembedahan mungkin diperlukan untuk membaiki katil kuku atau mengeluarkan tisu yang rosak.
Kesimpulan:
Trauma kuku boleh menyakitkan dan mengecewakan, tetapi terdapat banyak pilihan rawatan yang tersedia untuk menguruskan kecederaan ini. Di Straits Podiatry, kami pakar dalam pelbagai gangguan kuku, termasuk rawatan trauma kuku, dan kami berdedikasi untuk membantu pesakit kami mencapai kesihatan kaki yang optimum. Jika anda mengalami sebarang masalah kuku jari kaki, jangan teragak-agak untuk menghubungi kami untuk temujanji. Kami komited untuk menyediakan penjagaan podiatrik berkualiti tinggi kepada pesakit kami di Singapura.
Apakah aktiviti yang tersedia di Nail Trauma?
Berapa lama masa yang diambil untuk trauma kuku sembuh?
Masa penyembuhan untuk kecederaan kuku boleh berbeza-beza bergantung kepada keterukan kecederaan. Secara umum, ia mengambil masa kira-kira 3-6 bulan untuk kuku jari kaki baru berkembang sepenuhnya. Sekiranya katil kuku tidak rosak, kuku harus tumbuh semula secara normal. Walau bagaimanapun, jika katil kuku cedera, ia boleh mengambil masa yang lebih lama untuk kuku tumbuh semula dan boleh tumbuh semula dengan bentuk atau tekstur yang tidak teratur.
Bolehkah trauma kuku sembuh?
Ya, trauma kuku boleh sembuh. Tahap dan kelajuan penyembuhan bergantung kepada keterukan trauma. Kecederaan ringan seperti lebam atau luka kecil biasanya akan sembuh sendiri tanpa campur tangan perubatan. Walau bagaimanapun, jika kecederaan lebih teruk dan melibatkan katil kuku atau tisu sekitarnya, ia mungkin memerlukan rawatan perubatan.
Ubat mana yang terbaik untuk kecederaan kuku?
Untuk kecederaan kuku kecil, ubat penahan sakit di kaunter boleh membantu mengurangkan kesakitan dan bengkak. Salap antiseptik seperti betadine juga boleh digunakan untuk mencegah jangkitan. Dalam kes kecederaan atau jangkitan yang lebih teruk, antibiotik preskripsi atau ubat antikulat mungkin diperlukan. Doktor anda boleh menentukan rawatan trauma kuku terbaik berdasarkan keterukan kecederaan anda.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Patah kaki (pecah dalam tulang kaki) boleh menyakitkan dan melemahkan. Itulah sebabnya kami telah mengumpulkan panduan komprehensif ini untuk membantu anda memahami keretakan, bagaimana ia berlaku, pilihan rawatan patah kaki apa yang tersedia, dan apa yang boleh anda lakukan untuk mencegah dan menguruskannya.
Apakah Patah Tulang?
Patah tulang pada dasarnya adalah rehat dalam tulang. Keretakan boleh berkisar dari retakan garis rambut kecil hingga pecah teruk yang menghancurkan tulang menjadi beberapa keping. Keretakan boleh berlaku di mana-mana tulang di dalam badan, tetapi ia adalah yang paling biasa di lengan dan kaki.
Apa yang menyebabkan Patah Tulang?
Keretakan biasanya disebabkan oleh kesan atau trauma, seperti kejatuhan, kemalangan kereta, atau kecederaan sukan. Mereka juga boleh disebabkan oleh penggunaan berlebihan, seperti tekanan berulang pada tulang atau pendedahan yang berpanjangan kepada ubat-ubatan tertentu yang melemahkan tulang.
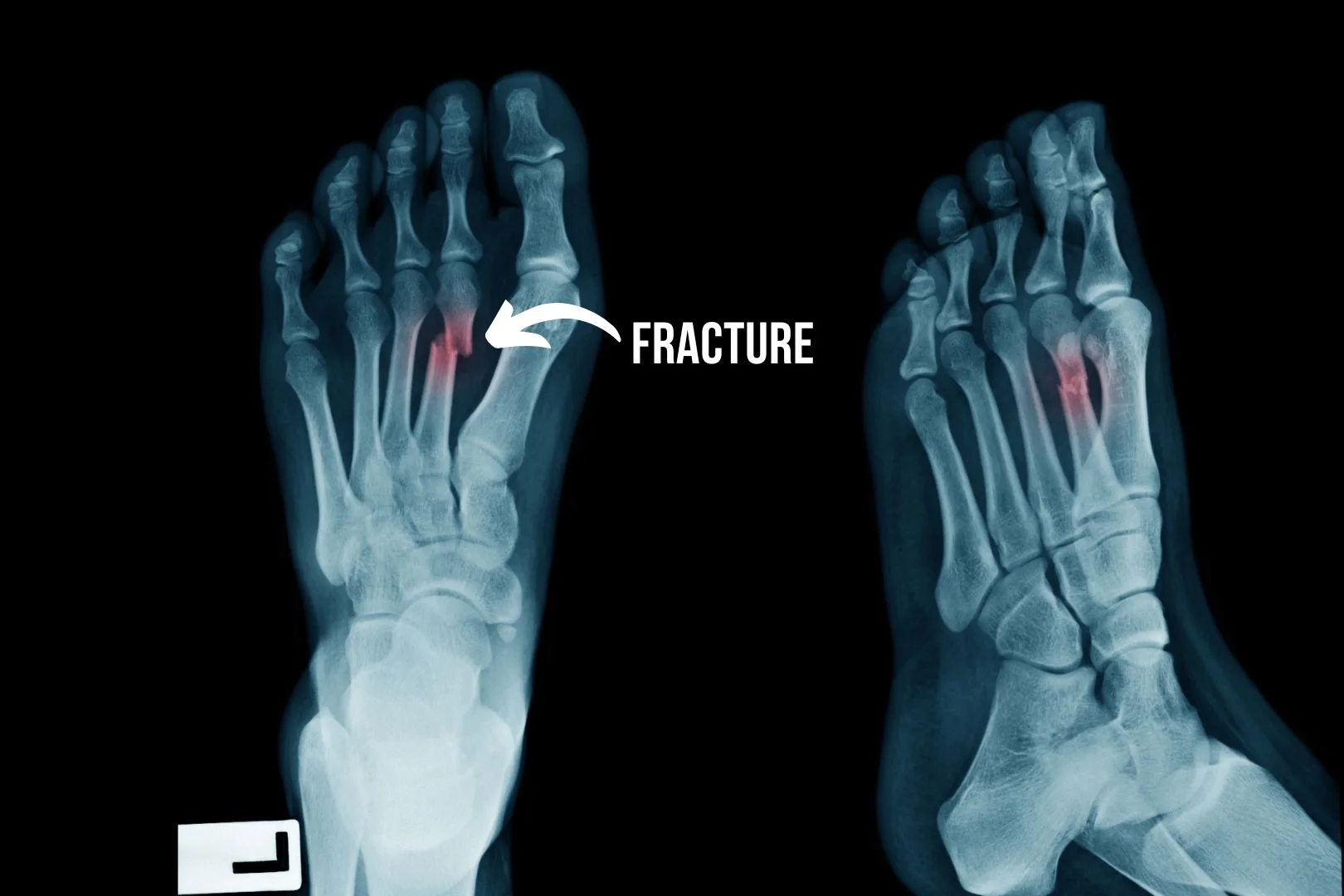
Jenis patah kaki
Terdapat beberapa jenis patah tulang, termasuk:
- Patah tertutup: Rehat tulang hadir, tetapi kulit utuh dan tiada luka terbuka.
- Patah terbuka: Tulang dan kulit pecah, yang boleh menyebabkan jangkitan.
- Patah hijau: Tulang sebahagiannya pecah di satu sisi, seperti tongkat patah, tetapi tidak sepenuhnya.
- Patah komaminuted: Tulang pecah atau hancur menjadi beberapa keping.
- Patah tekanan: Retak garis rambut kecil di tulang yang disebabkan oleh tekanan berulang.
- Patah avulsion: Cip di dalam tulang akibat daya tarikan tendon atau ligamen secara tiba-tiba, sering berlaku dalam terseliuh buku lali.
Gejala patah tulang
Gejala patah tulang boleh termasuk:
- Kesakitan di tapak patah tulang.
- Bengkak.
- Lebam.
- Kesukaran menggerakkan anggota yang terjejas.
- Kecacatan.
Pilihan Rawatan Patah Kaki di Singapura
Rawatan patah kaki berbeza-beza bergantung kepada keterukan patah tulang. Patah kaki kecil selalunya boleh bertambah baik dengan rehat, ais, mampatan, dan ketinggian (RICE). Patah kaki yang lebih teruk mungkin memerlukan rawatan, seperti imobilisasi dengan pelakon, pendakap, atau pembedahan.

Mencegah patah kaki
Terdapat beberapa perkara yang boleh anda lakukan untuk mengelakkan keretakan kaki, termasuk:
- Makan makanan yang sihat kaya dengan kalsium dan vitamin D.
- Mengambil bahagian dalam latihan menanggung berat.
- Memakai peralatan perlindungan semasa sukan berimpak tinggi atau bersentuhan dan aktiviti berisiko tinggi yang lain.
- Memakai kasut yang sesuai untuk aktiviti tersebut (contohnya kasut lari kusyen untuk maraton)
- Mengelakkan merokok dan pengambilan alkohol yang berlebihan.
Kenapa Pilih Straits Podiatry?
Di Straits Podiatry, kami pakar dalam menguruskan kecederaan kaki dan buku lali, termasuk rawatan patah kaki. Pasukan podiatrik berpengalaman kami akan menilai dan membangunkan pelan rawatan patah kaki yang sesuai yang memenuhi keperluan unik anda.
Hubungi Kami Hari Ini
Jangan tunggu untuk mendapatkan rawatan jika anda mengalami sakit kaki atau buku lali. Hubungi Straits Podiatry hari ini untuk menjadualkan temu janji dengan salah seorang pakar podiatrik kami yang berpengalaman.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Healthy feet are crucial for a fulfilling life, especially in a city like Singapore, where people are always on the move. Many people tend to neglect their feet until problems arise, but it’s essential to take good care of them to avoid pain, discomfort, and even injuries. In this article, we’ll share 5 top foot care tips that will help you maintain healthy and happy feet.
Foot Care Tips #1: Wear Proper Footwear
Wearing the right shoes is essential for maintaining good foot health. Your feet are the foundation of your body, and your shoes can either support or damage them. Here are some tips to help you choose and wear proper footwear:
- Proper fit: Check that your shoes fit properly. Blisters, calluses, and other foot problems can be caused by shoes that are too tight or loose. Get your feet measured regularly, as shoe sizes can change over time.
- Arch support: Look for shoes with good arch support. This is particularly critical if you have flat feet or high arches. Arch support can help prevent foot fatigue and alleviate pain in the feet, legs, and even lower back.
- Heel support: Make sure your shoes have proper heel support. Shoes with a flimsy or unstable heel can increase the risk of ankle sprains and other injuries. The heel should fit tightly in the shoe and not slip out.
- Sole thickness: Look for shoes with a thick, shock-absorbing sole. Thin soles can cause foot pain and increase your risk of foot injuries. A good sole should be flexible but provide enough support and protection for your feet. However, if you are elderly, thin soles will be better as they help you feel the ground better.
- Toe box: Choose shoes with a roomy toe box. A large toe box allows your toes to move freely and prevents cramped toes. Shoes that are too narrow can cause bunions and other foot deformities.
- Material: Look for shoes made of breathable materials like leather or mesh. This allows your feet to breathe and prevents moisture buildup. Avoid shoes made of synthetic materials that can trap heat and sweat.
- Activity-specific: Choose shoes based on the activity you will be doing. Running shoes are designed for running, while hiking boots are for hiking. Using the wrong shoes for an activity can increase your risk of foot injuries.

Foot Care Tips #2: Keep Your Feet Clean and Dry
When it comes to taking care of your body, one of the most overlooked parts is the feet. People often forget that the feet require attention, too. They are the foundation of your body, and if they are not taken care of properly, it can lead to various foot problems. One of the most essential things you can do to keep your feet healthy is to keep them clean and dry. Here are some tips to help you keep your feet clean and dry:
- Wash your feet daily: Use warm water and soap to wash your feet daily. Scrub your feet gently with a washcloth or sponge. Make sure your feet are thoroughly dry, especially between your toes.
- Wear clean socks: Always wear clean, dry socks. Avoid wearing the same pair of socks two days in a row. Choose socks that fit well and are made of breathable materials like cotton or wool.
- Wash your shoes: It’s essential to wash and clean your shoes regularly to avoid moisture buildup. Moisture is the perfect breeding ground for bacteria and fungi. Avoid wearing wet shoes, and make sure to let your shoes air out between uses.
- Keep your toenails trimmed: Trim your toenails straight across, and avoid cutting them too short. Use a clean, sharp nail clipper to prevent ingrown toenails and other foot problems.
- Use foot powder: Foot powder can help absorb moisture and prevent odour. Sprinkle a small amount of foot powder inside your shoes and on your feet before putting on your socks.
- Avoid walking barefoot: Walking barefoot in public places like locker rooms, swimming pools, and showers can expose your feet to fungus and bacteria. Always wear sandals or flip-flops to protect your feet.
- See a podiatrist: If you have persistent foot problems like athlete’s foot, toenail fungus, or warts, see a podiatrist. A podiatrist can provide you with the necessary treatment to get your feet healthy again.

Foot Care Tips #3: Trim Your Toenails Properly
Trimming your toenails might seem like a simple task, but it’s important to do it properly to avoid any foot-related issues. We recommend keeping your toenails trimmed regularly to prevent ingrown toenails, infection, and other foot problems.
- Start by washing your feet with soap and warm water to soften the nails, making it easier to trim them.
- Use clean and non-rusty tools. You can use toenail clippers or nail scissors, depending on your preference. Make sure to use a clean nail file to smooth the edges of the nails after trimming.
- Cut your nails straight across. Avoid cutting them too short or curved, as it can cause ingrown toenails. If you have thick nails, try thinning them by filing them before trimming.
- Avoid cutting the corners of your nails. This can also lead to ingrown toenails. Instead, use a nail file to round the edges gently.
- Take care of your cuticles. Please don’t cut them too much or too often, as they serve as a protective barrier against infection. You should also avoid pushing them back using a cuticle pusher.
- Practice good hygiene. After trimming your nails, clean your tools and wash your hands and feet thoroughly.
Foot Care Tips #4: Moisturize Your Feet Regularly
Moisturizing your feet is essential for maintaining good foot health. Neglecting your feet can lead to problems such as dry skin, cracked heels, calluses, and other foot conditions. Therefore, it’s vital to incorporate regular foot care into your daily routine.
One of the best ways to moisturize your feet is by applying a good quality moisturizing lotion or foot cream. Look for products that contain ingredients such as glycerin, shea butter, or urea, as these help to lock in moisture and keep your feet hydrated. Apply the lotion or cream on your feet after a shower or a foot soak when your skin is clean and pores are open.

Foot Care Tips #5: Stretch Your Feet and Ankles
Stretching your feet and ankles is crucial for maintaining good foot and ankle health. Tightness and immobility in the foot and ankle can lead to a variety of problems, such as plantar fasciitis, Achilles tendonitis, heel pain, and ankle sprains. Here are some simple yet effective stretches to improve your foot and ankle flexibility and mobility.
1. Toe Flexor Stretch: Sit on a chair and place a towel on the floor in front of you. Using your toes, scrunch up the towel towards you. Hold for a few seconds and release. Repeat 10-15 times.
2. Calf Stretch: Stand facing a wall and place your hands on the wall. Step back with one foot, keeping your heel on the ground. Lean forward until you feel a calf stretch. Hold for 20-30 seconds before switching sides.
3. Ankle Dorsiflexion Stretch: Sit on the ground with your legs straight out in front of you. Place a resistance band around the ball of one foot and hold onto the ends of the band. Gently move your foot towards you until your ankle stretches. Hold for 20-30 seconds before alternating sides.
4. Arch Stretch: Sit on a chair and place a tennis ball or a rolled-up towel under your foot arch. Roll your foot back and forth over the ball/towel for 1-2 minutes.
5. Plantar Fascia Stretch: Sit on a chair and place your foot on the other thigh. Bend the big toe of the foot upwards and pull the ankle towards the shin until you feel a stretch in the bottom of your foot. Hold for 20-30 seconds before switching sides.
In conclusion, stretching your feet and ankles is essential to maintaining good foot and ankle health. Incorporating the above-mentioned stretches into your daily routine can improve your foot and ankle mobility, flexibility, and stability.
Seek Help From Podiatrist When Necessary
We hope you have learned a lot from the above foot care tips! If you are experiencing any foot or ankle pain or discomfort, it is essential to consult a podiatrist for proper diagnosis and treatment. For residents of Singapore, Straits Podiatry offers expert podiatry services to help you address any foot or ankle issues you may be facing. Learn more about our services and schedule an appointment with our experienced podiatrists. Take the first step towards better foot and ankle health today.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Pengenalan
Tumit lebih daripada sekadar bahagian belakang kaki anda; Ia adalah struktur kompleks yang terdiri daripada pelbagai tulang, otot, ligamen, dan tendon. Memahami anatomi tumit boleh memberikan pandangan berharga mengenai keadaan seperti sakit tumit, fasciitis plantar, dan tendinitis Achilles. Artikel ini akan membimbing anda melalui komponen penting anatomi tumit.
Calcaneus: Asas Tumit
calcaneus, atau tulang tumit, adalah tulang terbesar di kaki. Ia berfungsi sebagai asas untuk bahagian belakang kaki dan memainkan peranan penting dalam berjalan dan berlari dengan menyediakan tuil untuk otot menggunakan kekuatan. Ia juga menanggung sebahagian besar beban badan kita semasa berjalan atau berlari, mengambil kesan dan tekanan yang tinggi setiap langkah yang kita ambil.
Ligamen dan Tendon
Terdapat dua struktur ligamentous dan tendinous utama yang melekat pada tulang tumit, dan mereka memainkan peranan penting dalam fungsi dan kestabilan kaki:
- Plantar Fascia: Jalur berserabut tebal tisu ini menghubungkan bahagian bawah tulang tumit ke jari kaki dan menyokong lengkungan kaki.
- Achilles Tendon: Tendon ini menghubungkan otot betis ke belakang tulang tumit dan penting untuk berlari, melompat, dan berdiri di jari kaki.
Otot yang Terlibat dalam Fungsi Tumit
Beberapa otot intrinsik berasal dari kawasan tumit. Mereka membantu tendon yang lebih besar dalam fungsi kaki:
- Quadratus Plantae: Membantu membantu flexor digitorium longus dalam flexing jari kaki yang lebih rendah
- Flexor Digitorum Brevis: Ini adalah otot sekunder yang membantu melenturkan jari kaki yang lebih rendah dan juga dianggap memberikan sokongan lengkungan.
- Abductor Hallucis: Salah satu otot yang lebih besar di kaki, terletak di kawasan gerbang. Ini membantu menculik dan melenturkan jari kaki besar dan memberikan kestabilan kaki.
- Abductor Digiti Minimi: Membantu menculik dan melenturkan jari kaki kecil. Otot yang tidak setiap individu boleh mengasingkan pengecutan dan pergerakannya.
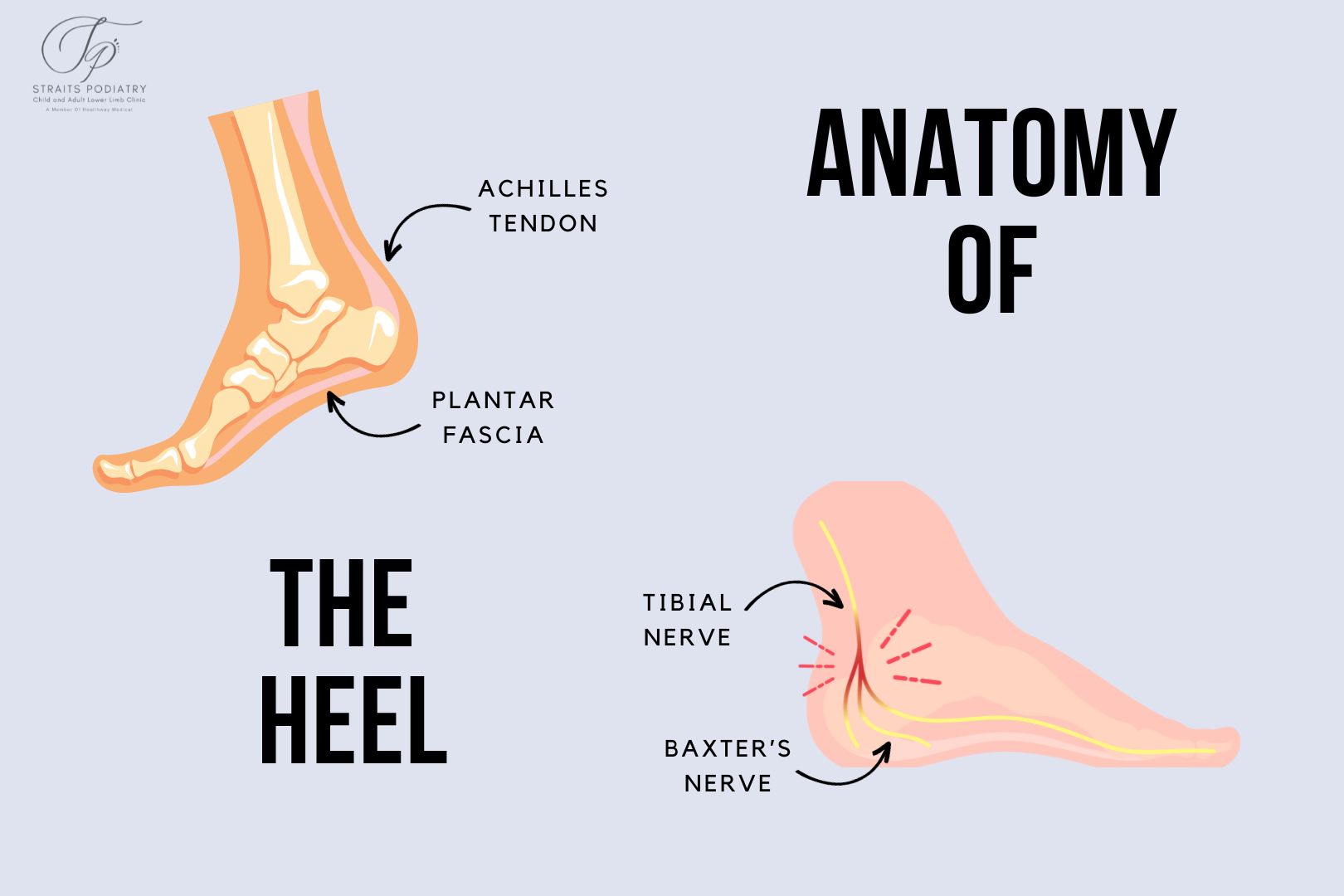
Tisu lembut dan saraf
Tisu lembut dan saraf dalam tumit memainkan peranan penting dalam mengurangkan kesan dan menyediakan kawalan deria motor masing-masing. Struktur utama ialah:
- Pad lemak: Struktur sarang lebah yang indah yang mengandungi tisu lemak yang terletak di bawah tulang tumit. Ia membantu menyerap kesan berjalan dan berlari.
- Saraf Tibial: Saraf terbesar masuk ke kaki. Saraf ini berjalan dari bahagian dalam buku lali ke bawah tumit dan boleh terlibat dalam keadaan seperti sindrom terowong tarsal.
- Saraf Baxter: Cawangan saraf yang berasal dari saraf plantar lateral. Mampatan saraf ini menyebabkan entrapment saraf Baxter.
Bagaimana Anatomi Menjejaskan Sakit Tumit
Memahami anatomi tumit boleh membantu profesional perubatan mendiagnosis dan merawat sakit tumit dengan lebih berkesan. Sebagai contoh, keradangan fascia plantar membawa kepada fasciitis plantar, manakala isu-isu dengan tendon Achilles boleh mengakibatkan tendinitis Achilles. Ia juga penting bagi profesional perubatan untuk mengetahui anatomi dengan baik untuk mentadbir rawatan kepada struktur yang betul.
Kesimpulan
Tumit adalah struktur yang kompleks dengan pelbagai komponen yang berfungsi dengan harmoni untuk membolehkan pergerakan dan memberikan sokongan dan kestabilan. Memahami anatominya boleh menawarkan pandangan berharga mengenai sebab-sebab dan rawatan keadaan yang berkaitan dengan tumit.
Artikel Berkaitan
- Sakit Tumit di Singapura - Memahami sebab-sebab, diagnosis, dan rawatan.
- Mengapa saya mengalami sakit tumit?
- Jenis gerbang kaki dan kesannya terhadap fasciitis plantar
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Pengenalan
Sakit tumit adalah isu biasa yang dihadapi oleh ramai rakyat Singapura, terutamanya memandangkan persekitaran bandar di negara ini. Gabungan perjalanan jauh, berjalan kaki yang luas, dan pilihan kasut boleh menyumbang kepada masalah ini. Melalui artikel ini, kami berhasrat untuk menyediakan perubahan gaya hidup praktikal untuk membantu anda mencegah atau mengurangkan sakit tumit dalam persekitaran bandar yang unik di Singapura.
Mengapa Sakit Tumit Menjadi Kebimbangan di Singapura?
Sakit tumit semakin biasa di Singapura kerana faktor-faktor seperti:
- Berjalan luas di permukaan keras seperti konkrit
- Kurang kesedaran tentang kepentingan kasut yang baik
- Budaya tidak pakai kasut di rumah ketika lantai jubin
- Kecenderungan umum untuk mengabaikan kesakitan di kaki
Berjalan Pintar
Salah satu cara yang paling mudah tetapi paling berkesan untuk mencegah sakit tumit adalah dengan berhati-hati dengan cara dan di mana anda berjalan. Berikut adalah beberapa petua:
- Pilih Laluan yang Betul: Elakkan permukaan keras semasa anda berjalan, terutamanya jika anda berkaki ayam.
- Fikiran Langkah Anda: Perhatikan gaya berjalan anda. Langkah yang seimbang dan sekata boleh mengurangkan tekanan pada tumit anda. Jika anda perlu berjalan pantas, berbuat demikian, tetapi ambil langkah yang lebih kecil. Overstriding boleh menyebabkan kesan tinggi berulang pada tumit anda.

Pilih kasut yang betul
Kasut memainkan peranan penting dalam mencegah sakit tumit. Berikut ialah perkara yang perlu dicari:
- Sokongan: Pastikan kasut anda mempunyai sokongan yang baik untuk lengkungan dan tumit untuk mengagihkan berat badan secara sama rata.
- Kusyen: Pilih kasut dengan kusyen yang mencukupi, terutamanya di sekitar kawasan tumit. Ambil perhatian bahawa kusyen tidak sama dengan fleksibiliti. Kasut hendaklah lembut tetapi tidak mudah dilenturkan ke semua arah.
- Patut: Pastikan kasut anda sesuai dengan baik. Kasut longgar atau ketat boleh menyumbang kepada sakit tumit.
Anda juga harus memilih kasut yang betul berdasarkan jenis kaki anda.
Menggabungkan Latihan Kaki
Senaman kaki yang kerap boleh membantu menguatkan otot dan ligamen di sekitar tumit anda, mengurangkan risiko sakit tumit. Beberapa latihan yang berkesan termasuk:
- Kenaikan Tumit: Berdiri rata di atas tanah dan angkat tumit anda, memegang selama beberapa saat.
- Keriting tuala: Semasa duduk, letakkan tuala di lantai dan gulung tuala menggunakan jari kaki anda.
Regangan Harian
Percaya atau tidak, kebanyakan orang melupakan kerja pemulihan. Kami menghabiskan berjam-jam setiap hari untuk otot kita, dan mereka akan menjadi tegang dari masa ke masa. Peningkatan ketegangan akan memberi tekanan kepada tendon dan fascia kita, yang boleh menyebabkan Achilles tendinitis dan fasciitis plantar. Oleh itu, adalah penting bahawa kita menghabiskan 5 hingga 10 minit setiap satu untuk melakukan satu siri regangan untuk meningkatkan fleksibiliti mereka. Ia sentiasa baik untuk melakukan regangan otot betis, hamstring, dan glute pada akhir setiap hari.
Kesimpulan
Sakit tumit di Singapura adalah kebimbangan yang semakin meningkat, sebahagian besarnya disebabkan oleh gaya hidup bandar kita. Walau bagaimanapun, dengan beberapa perubahan gaya hidup praktikal, anda boleh mengurangkan risiko anda dengan ketara. Daripada berjalan dengan bijak hingga memilih kasut yang betul dan menggabungkan senaman kaki, petua ini boleh pergi jauh dalam memastikan tumit anda sihat.
Artikel Berkaitan
- Latihan Fasciitis Plantar: Panduan Langkah demi Langkah
- Bagaimana Untuk Memilih Kasut Yang Sesuai Untuk Kaki Saya?
- Jenis gerbang kaki dan kesannya terhadap fasciitis plantar
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Pengenalan
Jenis gerbang kaki dengan ketara menentukan kerentanan dan risiko anda terhadap pelbagai keadaan kaki, termasuk fasciitis plantar. Memahami lengkungan kaki anda boleh memberikan pandangan berharga tentang mengapa anda mungkin mengalami sakit tumit dan cara terbaik untuk menguruskannya. Artikel ini akan meneroka pelbagai jenis gerbang kaki, ciri-ciri mereka, dan kesannya terhadap fasciitis plantar.
Jenis Gerbang Kaki
1. Gerbang Biasa
- Ciri-ciri: Gerbang seimbang kelihatan pada mata, biasanya pengagihan berat badan yang sekata.
- Kesan ke atas Plantar Fasciitis: Individu yang mempunyai gerbang normal mempunyai risiko yang lebih rendah untuk membangunkan fasciitis plantar. Penjajaran dan pengagihan berat badan yang betul membantu mengurangkan tekanan yang tidak wajar pada fascia plantar. Kecederaan biasanya berlaku kerana pilihan kasut atau aktiviti fizikal yang lemah.
2. Kaki Rata (Gerbang Rendah)
- Ciri-ciri: Gerbang duduk rendah, hampir sepenuhnya atau sepenuhnya rata ke tanah. Tumit juga condong ke dalam dari pandangan belakang.
- Kesan pada Plantar Fasciitis: Kaki rata cenderung menyebabkan pergelangan kaki ke dalam, yang dikenali sebagai overpronation. Ini boleh meletakkan ketegangan tambahan dan meregangkan fascia plantar, menjadikan individu lebih mudah terdedah kepada fasciitis plantar.
3. Gerbang Tinggi
- Ciri-ciri: Gerbang tinggi, beban berlebihan pada bola dan tumit kaki.
- Kesan ke atas Fasciitis Plantar: Gerbang tinggi boleh menyebabkan kekurangan atau supinasi, mengehadkan keupayaan badan untuk menyerap kejutan apabila berjalan atau berlari. Ini boleh menyebabkan tekanan pada plantar fascia, yang membawa kepada fasciitis plantar.

Cara Menentukan Jenis Gerbang Anda
1. Ujian Jejak Basah
Cara paling mudah untuk menentukan jenis gerbang anda ialah ujian basah. Basahkan tapak kaki anda, kemudian melangkah ke permukaan yang kering dan rata. Tapak kaki yang ditinggalkan akan memberikan petunjuk jenis gerbang anda.
2. Penilaian Profesional
Berunding dengan podiatrist untuk penilaian kaki yang komprehensif pastinya merupakan cara yang paling tepat untuk menentukan jenis lengkungan anda dan implikasinya untuk kesihatan kaki anda.
Menguruskan Fasciitis Plantar Berdasarkan Jenis Gerbang
Kaki Rata
- Insoles Ortotik: Ortotik tersuai boleh memberikan sokongan yang diperlukan untuk membantu membetulkan overpronation dan mengurangkan ketegangan pada fascia plantar.
- Kasut Kestabilan: Kasut dengan kawalan pronasi terbina dalam boleh memberi manfaat.
Gerbang Tinggi
- Insoles kusyen: Gerbang tinggi memerlukan kusyen untuk mengimbangi titik tekanan pada kaki.
- Kasut Menyerap Kejutan: Kasut dengan kusyen yang baik boleh membantu menguruskan ketidakselesaan yang berkaitan dengan lengkungan tinggi.
Gerbang Biasa
- Pemeriksaan Kasut Biasa: Pastikan kasut anda berada dalam keadaan baik dan menawarkan sokongan yang mencukupi.
- Latihan Pencegahan: Rutin regangan dan latihan pengukuhan dapat membantu mengekalkan kesihatan kaki. Jika anda suka berlari, adalah penting untuk mempelajari petua untuk mengelakkan kecederaan lari.
Kesimpulan
Memahami jenis gerbang kaki anda berguna dalam pencegahan dan pengurusan fasciitis plantar. Memilih pilihan kasut dan ortotik yang betul berdasarkan jenis lengkungan anda boleh membantu memberikan kelegaan yang ketara dan mengurangkan risiko mengalami keadaan yang menyakitkan ini.
Melengkapkan diri anda dengan pengetahuan tentang jenis gerbang anda dan kesannya boleh menjadi langkah pertama ke arah rawatan dan pencegahan fasciitis plantar yang berkesan. Sekiranya anda tidak pasti tentang jenis kaki anda, sila berunding dengan kami atau penyedia penjagaan kesihatan untuk penilaian kaki yang komprehensif hari ini.
Bacaan lanjut
- Plantar Fasciitis – Panduan komprehensif untuk memahami fasciitis plantar.
- Peranan Terapi Shockwave dalam Rawatan Fasciitis Plantar - Ketahui bagaimana terapi gelombang kejutan boleh menjadi rawatan yang berkesan untuk fasciitis plantar.
- Latihan Fasciitis Plantar: Panduan Langkah demi Langkah - Latihan praktikal untuk mengurus dan mencegah fasciitis plantar.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Pengenalan
Plantar fasciitis adalah keadaan melemahkan yang menyebabkan sakit tumit yang tajam dan sengit, sering membuat aktiviti mudah seperti berjalan mencabar. Bagi mereka yang tidak menemui kelegaan daripada rawatan konservatif seperti ortotik, senaman regangan, atau ubat-ubatan, terapi gelombang kejutan muncul sebagai penyelesaian yang menjanjikan. Dalam artikel ini, kami akan melalui peranan Terapi Shockwave Extracorporeal (ESWT) dalam menyokong rawatan fasciitis plantar, keberkesanannya, dan apa yang boleh anda harapkan jika anda memilih kaedah rawatan ini.
Apakah Terapi Shockwave?
Terapi Shockwave Extracorporeal (ESWT) adalah kaedah rawatan tidak invasif yang menggunakan gelombang kejutan untuk merangsang penyembuhan dalam tisu yang terjejas. Terapi ini melibatkan menyampaikan gelombang kejutan akustik kepada fascia plantar yang meradang untuk meningkatkan peredaran darah dan mempercepatkan proses penyembuhan semula jadi badan.
Bagaimana Terapi Shockwave Berfungsi?
Prinsip di sebalik ESWT adalah untuk merangsang microtrauma dalam tisu yang meradang. Mikrotrauma ini memulakan tindak balas keradangan, yang membawa kepada pembentukan saluran darah baru, peningkatan penghantaran nutrien, dan, akhirnya, penyembuhan fascia plantar yang lebih cepat. Terapi ini juga boleh merangsang pertumbuhan semula sel, membubarkan tisu parut, dan melegakan kesakitan dengan mengubah impuls saraf.
Keberkesanan Terapi Shockwave untuk Fasciitis Plantar
Beberapa kajian telah menunjukkan keberkesanan ESWT dalam merawat fasciitis plantar:
- Melegakan Kesakitan: Beberapa kajian membuktikan bahawa kebanyakan pesakit melaporkan pengurangan kesakitan yang ketara selepas menjalani rawatan ESWT. 1,2 Kursus rawatan biasanya melibatkan antara 4 hingga 6 sesi.
- Peningkatan dalam Mobiliti: Pengurangan kesakitan membolehkan pesakit merasa lebih mudah untuk melakukan latihan pemulihan lain, membantu pemulihan yang lebih cepat.
- Manfaat Jangka Panjang: Kajian telah menunjukkan bahawa terapi gelombang kejutan memberikan kelegaan jangka panjang dan oleh itu dianggap sebagai penyelesaian jangka panjang. 3
- Kesan Sampingan Minimum: ESWT tidak invasif dan secara amnya selamat, dengan kesan sampingan yang minimum seperti sedikit ketidakselesaan atau lebam di tapak rawatan.
Siapa yang boleh mendapat faedah?
Terapi gelombang kejutan biasanya disyorkan untuk pesakit yang:
- Telah didiagnosis dengan fasciitis plantar
- Mempunyai kemerosotan ketara plantar fascia
- Tidak bertindak balas dengan baik terhadap kaedah rawatan tradisional seperti ubat-ubatan, regangan, dan pengukuhan.
Apakah Prosedur Rawatan?
Prosedur ESWT pada dasarnya adalah rawatan pesakit luar yang biasanya mengambil masa kira-kira 20-30 minit. Langkah-langkahnya adalah seperti berikut:
- Perundingan Awal: Penilaian menyeluruh terhadap keadaan anda dan sejarah perubatan asas diperlukan untuk menentukan sama ada ESWT sesuai untuk anda.
- Pengimejan diagnostik: Adalah penting untuk mempunyai visualisasi yang jelas tentang plantar fascia, sama ada melalui ultrasound diagnostik atau MRI, untuk memastikan diagnosis itu tepat sebelum rawatan
- Penyediaan: Kawasan rawatan dibersihkan terlebih dahulu, dan gel digunakan untuk memudahkan aplikasi gelombang kejutan.
- Penghantaran Shockwave: Peranti pegang tangan menyampaikan gelombang kejutan akustik ke kawasan yang disasarkan. Anda biasanya akan mengalami sensasi mengetuk atau membosankan semasa rawatan.
- Selepas rawatan: Selepas rawatan, pesakit biasanya boleh meneruskan aktiviti normal mereka, walaupun latihan berat harus dielakkan selama beberapa minggu.
Kesimpulan
Terapi shockwave membentangkan pilihan rawatan plantar fasciitis yang menarik, terutamanya bagi mereka yang mempunyai kes kronik yang tidak bertindak balas dengan baik terhadap kaedah tradisional. Dengan manfaat yang ketara dalam melegakan kesakitan dan mobiliti, ditambah pula dengan kesan sampingan yang minimum, ESWT mungkin merupakan rawatan yang anda cari.
Kami berharap dengan menggabungkan maklumat berharga ini ke dalam perjalanan penjagaan kesihatan anda, anda boleh membuat keputusan yang tepat mengenai pengurusan fasciitis plantar dengan berkesan. Jangan ragu untuk berunding dengan kami atau penyedia penjagaan kesihatan anda untuk menentukan sama ada terapi gelombang kejutan sesuai untuk anda.
Bacaan lanjut
- Plantar Fasciitis – Panduan komprehensif untuk memahami plantar fasciitis, gejala-gejala, dan kaedah rawatan yang ada.
- Jenis Gerbang Kaki dan Kesannya terhadap Fasciitis Plantar - Membincangkan bagaimana jenis lengkungan kaki yang berbeza dapat menyumbang kepada fasciitis plantar.
- Latihan Plantar Fasciitis: Panduan Langkah demi Langkah - Menyediakan latihan regangan dan pengukuhan untuk mengurus dan mencegah fasciitis plantar.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Rujukan
- Melese H, Alamer A, Getie K, Nigussie F, Ayhualem S. Extracorporeal terapi gelombang kejutan mengenai fungsi sakit dan kaki dalam subjek dengan fasciitis plantar kronik: ulasan sistematik kajian terkawal rawak. Disabil Rehabil. 2022 Sep; 44(18):5007-5014. DOI: 10.1080/09638288.2021.1928775. Epub 2021 Mei 26. PMID: 34038642.
- Gollwitzer H, Saxena A, DiDomenico LA, et al. (2015). Keberkesanan klinikal yang relevan bagi terapi gelombang kejutan extracorporeal yang tertumpu dalam rawatan fasciitis plantar kronik: kajian multicenter rawak terkawal. Jurnal Pembedahan Tulang dan Sendi, 97(9), 701-708.
- Wang C-J, Wang F-S, Yang KD, Weng L-H, Ko J-Y. Keputusan jangka panjang Rawatan Extracorporeal Shockwave untuk Fasciitis Plantar. Jurnal Perubatan Sukan Amerika. 2006; 34(4):592-596. doi:10.1177/0363546505281811
Pengenalan
Fasciitis plantar boleh mengubah walaupun aktiviti paling mudah menjadi usaha yang menyakitkan. Mujurlah, latihan yang disasarkan dapat membantu mengurangkan kesakitan dan bahkan mencegah keadaan menjadi lebih teruk. Panduan langkah demi langkah ini bertujuan untuk memberi anda satu set latihan untuk mengurus dan berpotensi melegakan gejala fasciitis plantar.
Mengapa Senaman Membantu
Melibatkan diri dalam senaman tertentu boleh membantu meningkatkan fleksibiliti dan kekuatan otot kaki dan betis anda, dengan itu mengurangkan ketegangan pada fascia plantar anda. Latihan ini bertujuan untuk:
- Regangkan tendon Achilles dan otot betis.
- Menguatkan otot di kaki anda.
- Meningkatkan keseimbangan dan kestabilan.
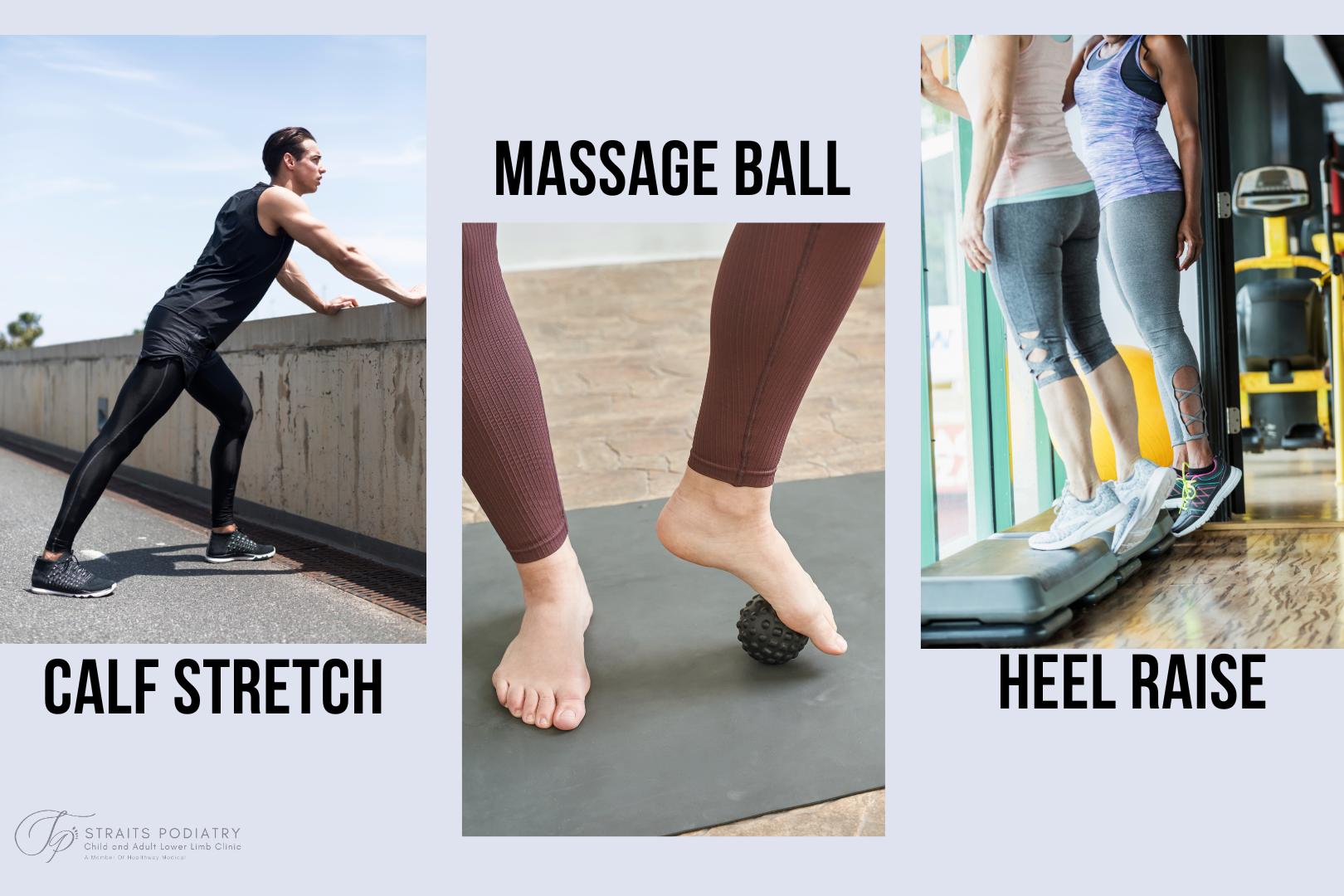
Latihan Fasis Plantar
1. Regangan Anak Lembu
Langkah-langkah:
- Berdiri menghadap dinding dengan tangan anda ditekan ke atasnya.
- Langkah satu kaki ke belakang, pastikan ia lurus.
- Bengkokkan lutut depan anda sambil mengekalkan tumit belakang anda di atas tanah.
- Tahan selama 20-30 saat, kemudian tukar sisi.
2. Regangan Plantar Fascia
Langkah-langkah:
- Duduk dan panjangkan kaki yang terjejas di hadapan anda.
- Ambil jari kaki anda dan perlahan-lahan tarik mereka ke arah anda.
- Pegang regangan selama 20-30 saat.
- Lakukan 3 set sekurang-kurangnya 2 kali sehari.
3. Keriting Tuala
Langkah-langkah:
- Duduk di atas kerusi dan letakkan tuala di bawah kaki anda.
- Gunakan jari kaki anda untuk mencungkil tuala ke arah anda.
- Ulangi untuk 10-15 rep.
4. Gulung Bola Urut
Langkah-langkah:
- Duduk di atas kerusi dan letakkan bola urut atau penggelek buih di bawah lengkungan anda.
- Gulung kaki anda berulang-alik ke atas.
- Lakukan selama 20-30 saat.
- Ulangi dua kali
5. Menaikkan Tumit
Langkah-langkah:
- Berdiri di belakang kerusi untuk sokongan.
- Naikkan tumit anda dari tanah, angkat ke jari kaki anda.
- Turunkan ke bawah perlahan-lahan dalam kiraan 5 saat.
- Adakah 10-15 wakil untuk 2 set.
Bila hendak melakukan latihan ini
Kami menasihati anda untuk berunding dengan pakar podiatrist atau penyedia penjagaan kesihatan sebelum memulakan sebarang rutin senaman. Ini adalah untuk memastikan bahawa anda mempunyai diagnosis yang jelas sebelum memulakan pengurusan anda. Setelah dibersihkan, anda boleh melakukan latihan ini setiap hari. Ingat, konsistensi adalah kunci.
Jaga
- Sentiasa memanaskan badan sebelum anda bermula.
- Hentikan sebarang senaman jika anda mengalami kesakitan atau ketidakselesaan.
- Rujuk penyedia penjagaan kesihatan untuk nasihat peribadi.
Kesimpulan
Senaman boleh memainkan peranan penting dalam mengurangkan gejala plantar fasciitis dan meningkatkan kesihatan kaki. Amalan yang konsisten ditambah dengan kasut yang betul dan rawatan lain boleh menetapkan anda di jalan menuju pemulihan.
Senaman yang konsisten boleh membawa kepada kelegaan yang berkekalan daripada fasciitis plantar. Sentiasa berunding dengan pembekal penjagaan kesihatan anda untuk diagnosis dan pilihan rawatan plantar fasciitis yang disesuaikan.
Bacaan lanjut
- Plantar Fasciitis – Panduan komprehensif mengenai sebab-sebab, diagnosis, dan rawatan plantar fasciitis
- Peranan Terapi Shockwave dalam Rawatan Fasciitis Plantar
- Jenis gerbang kaki dan kesannya terhadap fasciitis plantar
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Rujukan
- DiGiovanni BF, Nawoczenski DA, DP Melayu, et al. (2006). Senaman regangan khusus Plantar fascia meningkatkan hasil pada pesakit dengan fasciitis plantar kronik. Jurnal Pembedahan Tulang dan Sendi, 88(8), 1775-1781.
- Martin JE, Hosch JC, Goforth WP, et al. (2001). Rawatan mekanikal fasciitis plantar: Satu kajian prospektif. Jurnal Persatuan Perubatan Podiatrik Amerika, 91(2), 55-62.
Sebagai satu pasukan podiatrists berpengalaman di Singapura, kita tahu bahawa metatarsus adductus adalah keadaan yang menjejas ramai orang tetapi jarang dibincangkan. Oleh itu, kami berada di sini untuk membantu anda memahaminya dengan lebih baik. Dalam artikel ini, kami akan membincangkan semua yang anda perlu tahu tentang metatarsus adductus, termasuk sebab, gejala, dan pilihan rawatan.
Apa itu Metatarsus Adductus?
Metatarsus adductus adalah keadaan kaki biasa yang mempengaruhi cara bahagian depan kaki (kaki depan) diletakkan. Keadaan ini menyebabkan lengkung di bahagian tengah kaki, menyebabkan bahagian depan kaki berpusing ke dalam. Lengkung masuk ini dikenali sebagai bentuk "C", yang memberikan kaki penampilan melengkung.
Kecacatan kaki ke dalam menyebabkan kanak-kanak atau orang dewasa berjalan dengan corak berjalan kaki kaki . Oleh itu, adalah penting untuk memeriksa adductus metatarsus apabila memeriksa seseorang dengan gaya berjalan kaki.
Metatarsus adductus boleh hadir semasa lahir, atau berkembang sebagai umur kanak-kanak. Keterukan keadaan boleh berkisar dari ringan hingga teruk, dan pelan rawatan bergantung kepada keterukan lengkung.
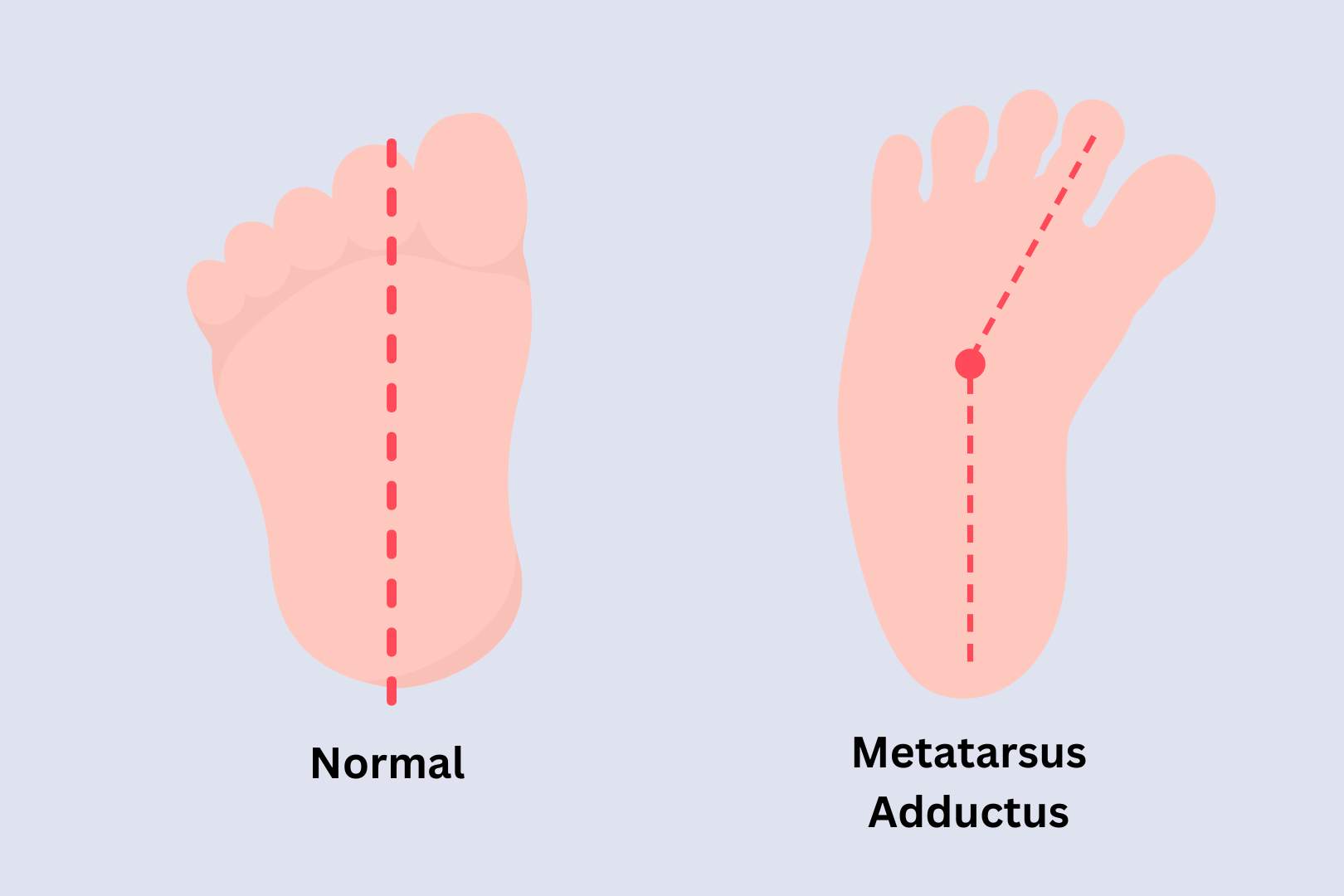
Diagnosis
Profesional perubatan atau podiatrist anda boleh mengenal pasti metatarsus adductus dengan mudah melalui pengusiran mudah, yang dikenali sebagai ujian Bleck. Sistem klasifikasi Bleck juga boleh membantu menentukan keterukan keadaan, dan jika keadaan itu boleh diperbetulkan.
X-ray adalah alat lain yang boleh membantu mengesan keadaan ini, tetapi secara amnya tidak diperlukan. Ini hanya perlu jika syarat itu menunjukkan kecacatan tetap, atau untuk menolak syarat-syarat seperti kaki skew atau kaki kelab.
Menyebabkan
Penyebab sebenar metatarsus adductus tidak jelas, tetapi kajian menunjukkan bahawa ia mungkin disebabkan oleh kedudukan bayi dalam rahim. Beberapa faktor yang boleh meningkatkan risiko keadaan ini termasuk:
- Sejarah keluarga: Jika seseorang dalam keluarga anda mempunyai metatarsus adductus, anda mungkin lebih cenderung untuk membangunkan keadaan ini.
- Anak sulung: Ia lebih biasa pada kanak-kanak yang dilahirkan pertama.
- Kedudukan breech: Bayi yang berada dalam kedudukan breech dalam rahim mungkin berisiko lebih tinggi untuk mengalami kecacatan kaki ini.
- Kembar: Metatarsus adductus kelihatan lebih kerap dalam kembar daripada kelahiran tunggal
Gejala-gejala
Gejala metatarsus adductus yang paling biasa adalah penampilan melengkung bahagian depan kaki. Gejala-gejala lain mungkin termasuk:
- Kesukaran memasang kasut dengan betul
- Kesakitan atau ketidakselesaan di kaki
- Mengurangkan fleksibiliti di kaki
- Kesukaran berjalan atau berdiri untuk tempoh yang panjang
Pilihan Rawatan untuk Metatarsus Adductus
Metatarsus adductus pada masa dewasa biasanya tidak boleh diperbetulkan tanpa sebarang pembedahan. Dalam kebudak-budakan, rawatan akan bergantung kepada keterukan keadaan. Dalam kes-kes ringan, keadaan ini boleh bertambah baik dengan sendirinya apabila kanak-kanak tumbuh. Walau bagaimanapun, dalam kes-kes yang lebih teruk, rawatan diperlukan untuk mengelakkan masalah kaki masa depan.
Antara pilihan rawatan di Singapura termasuklah:
- Latihan regangan: Senaman regangan yang kerap boleh membantu meningkatkan fleksibiliti di kaki.
- Kasut khas: Dalam sesetengah kes, kasut khas, pendakap kaki pediatrik , atau ortos kaki mungkin diperlukan untuk menyokong kaki dan menggalakkan perkembangan yang betul.
- Pemutus bersiri: Dalam kes yang lebih teruk, pemutus mungkin diperlukan untuk membetulkan kedudukan kaki.
- Pembedahan: Dalam kes-kes yang jarang berlaku, membetulkan kedudukan kaki melalui pembedahan mungkin diperlukan.
Adakah Metatarsus Adductus hilang?
Dalam sesetengah kes, metatarsus adductus boleh menyelesaikan sendiri apabila kanak-kanak tumbuh dan mula berjalan lebih banyak. Walau bagaimanapun, dalam kes lain, keadaan ini mungkin berterusan atau bertambah buruk dari masa ke masa, yang membawa kepada masalah kaki yang lain. Kemungkinan metatarsus adductus akan hilang bergantung kepada keterukan keadaan dan umur kanak-kanak. Adalah penting untuk memantau perkembangan kaki kanak-kanak dan mendapatkan rawatan perubatan jika terdapat sebarang kebimbangan.
Bolehkah Metatarsus Adductus Menjejaskan Berjalan?
Adductus metatarsus boleh menjejaskan cara kanak-kanak berjalan, kerana ia boleh menyebabkan kaki berpusing ke dalam dan menjejaskan keseimbangan dan kestabilan kaki. Kanak-kanak dengan keadaan ini mungkin mempunyai corak berjalan kaki dan mungkin lebih terdedah kepada tersandung atau tersandung. Walau bagaimanapun, dengan rawatan dan pengurusan yang sesuai, kebanyakan kanak-kanak boleh berjalan dan berjalan seperti biasa.
Adakah Metatarsus Adductus membetulkan dirinya sendiri?
Dalam sesetengah kes, ia boleh membetulkan dirinya dari masa ke masa apabila kanak-kanak tumbuh dan berkembang. Walau bagaimanapun, ini tidak selalu berlaku, dan sesetengah kanak-kanak mungkin memerlukan rawatan untuk mengelakkan masalah kaki yang lain daripada berkembang. Pengesanan dan pengurusan awal sering membawa kepada peluang yang lebih baik untuk hasil yang berjaya.
Apakah Kesan Jangka Panjang Metatarsus Adductus?
Keadaan ini boleh membawa kepada masalah kaki yang lain jika mereka berterusan melalui kehidupan, seperti metatarsalgia, hammertoes, dan bunion tukang jahit. Keadaan ini biasanya menyebabkan kesakitan, ketidakselesaan, dan kesukaran berjalan atau berdiri. Di samping itu, kanak-kanak dengan metatarsus adductus mungkin sukar untuk mengambil bahagian dalam sukan, terutamanya jika kestabilan mereka terjejas. Oleh itu, adalah penting untuk memantau perkembangan kaki kanak-kanak dan mendapatkan rawatan yang sesuai jika diperlukan.
Kesimpulan
Metatarsus adductus adalah keadaan kaki biasa yang boleh menyebabkan ketidakselesaan dan kesukaran berjalan. Di Straits Podiatry, kami berada di sini untuk membantu anda memahami keadaan ini dengan lebih baik dan memberikan anda pilihan pengurusan yang terbaik. Jika anda atau seseorang yang anda kenali mengalami gejala di atas, sila jangan teragak-agak untuk menghubungi kami untuk berunding. Pasukan podiatrik berpengalaman kami ada di sini untuk membantu anda setiap langkah.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Clubfoot adalah keadaan kaki pediatrik kongenital yang mempengaruhi perkembangan kaki bayi. Ia menyebabkan satu atau kedua-dua kaki berpusing ke dalam dan ke bawah. Walaupun punca sebenar clubfoot tidak diketahui, ia dipercayai gabungan faktor genetik dan persekitaran. Keadaan ini boleh didiagnosis melalui pemeriksaan fizikal oleh pakar bedah podiatrist atau ortopedik.
Di Straits Podiatry, kami memahami kesan yang boleh dialami oleh kelab terhadap kehidupan kanak-kanak, dan kami ingin memberikan ibu bapa maklumat yang mereka perlukan untuk membuat keputusan termaklum mengenai kesihatan anak mereka. Dalam artikel ini, kami akan menyediakan panduan komprehensif untuk clubfoot, sebab, diagnosis, dan pilihan rawatan.
Apa itu Clubfoot?
Kaki kelab, atau talipes equinovarus, ialah gangguan kongenital yang menjejaskan satu atau kedua-dua kaki bayi baru lahir. Ia adalah kecacatan kaki yang agak jarang berlaku yang berlaku dalam kira-kira 1 dalam 1,000 kelahiran. Kaki kelab menyebabkan kaki atau kaki bayi berpusing ke dalam dan ke bawah, menyukarkan berjalan dan memakai kasut. Ia adalah keadaan yang tidak mengancam nyawa tetapi boleh melemahkan dengan teruk tanpa rawatan awal. Keadaan ini tidak boleh dikelirukan dengan berjalan kaki atau metatarsus adductus, di mana hanya kaki berpusing ke dalam apabila kanak-kanak berjalan.
Terdapat dua jenis utama kaki kelab: idiopatik dan bukan idiopatik. Idiopathic clubfoot adalah jenis yang paling biasa, dan puncanya tidak diketahui. Clubfoot bukan idiopatik boleh disebabkan oleh faktor-faktor lain, seperti keadaan neurogenik, myogenic, atau arthrogrypotic. Terlepas dari jenisnya, diagnosis dan rawatan awal adalah penting untuk hasil yang terbaik.
Menyebabkan
Punca sebenar tidak diketahui, tetapi ia dipercayai gabungan faktor genetik dan persekitaran. Kajian telah menunjukkan bahawa jika satu atau kedua-dua ibu bapa mempunyai kaki kelab, peluang anak mereka untuk dilahirkan dengan keadaan ini meningkat dengan ketara. Faktor risiko lain termasuk:
- Kelahiran pramatang
- Tahap cecair amniotik yang rendah
- Kedudukan bayi dalam rahim
- Gangguan neurologi
Diagnosis
Clubfoot umumnya ketara semasa lahir kerana penampilannya yang berbeza. Doktor biasanya akan merujuk anak anda kepada doktor ortopedik untuk menentukan keterukan keadaan. Mereka juga boleh memerintahkan X-ray atau ultrasound untuk menilai tulang dan sendi di kaki.
Rawatan
Rawatan clubfoot bergantung kepada keterukan keadaan. Dalam kes ringan, podiatrist boleh mengesyorkan latihan regangan, kaki dan pendakap buku lali, dan satu siri pelakon untuk secara beransur-ansur menggerakkan kaki ke kedudukan yang betul. Dalam kes-kes yang lebih teruk, pembedahan hampir selalu diperlukan untuk membetulkan kecacatan. Selepas rawatan, kanak-kanak perlu memakai kasut atau pendakap khas untuk mengekalkan kedudukan kaki yang betul selama beberapa tahun.
Kesimpulan
Clubfoot boleh melemahkan teruk jika dibiarkan tanpa rawatan awal. Walaupun doktor biasanya menyedari keadaan semasa lahir, beberapa kes ringan akan terlalu sukar untuk dikesan. Anda harus membawa anak anda ke profesional perubatan jika anda mengesyaki dia mempunyai keadaan. Ingat, diagnosis dan rawatan awal sangat penting untuk memastikan hasil terbaik untuk kesihatan kaki anak anda.
Soalan lazim:
Adakah Clubfoot kelainan kongenital?
Ya, kaki kelab adalah keabnormalan kongenital. Ini bermakna ia hadir semasa lahir dan menjejaskan perkembangan kaki. Kaki kelab adalah kecacatan yang agak jarang berlaku, dengan insiden sekitar 1 dalam 1,000 kelahiran. Ia dicirikan oleh pusingan ke dalam dan ke bawah satu atau kedua-dua kaki, menyukarkan kanak-kanak untuk berjalan dan memakai kasut.
Adakah Clubfoot Diwarisi?
Clubfoot dipercayai kongenital dan diwarisi. Kajian telah menunjukkan bahawa jika satu atau kedua-dua ibu bapa mempunyai kaki kelab, peluang anak mereka untuk dilahirkan dengan keadaan ini meningkat dengan ketara. Risiko mempunyai anak dengan kaki kelab adalah sekitar 1 dalam 30 jika salah seorang ibu bapa mempunyai keadaan dan 1 dalam 3 jika kedua-dua ibu bapa memilikinya. Walau bagaimanapun, adalah penting untuk diperhatikan bahawa tidak semua kes clubfoot adalah hasil daripada sejarah keluarga, dan etiologi spesifik keadaan masih belum diketahui.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Apakah Sindrom Curly Toe?
Sindrom Curly Toe adalah keadaan kaki biasa yang menjejas ramai orang di Singapura. Ia adalah kecacatan yang menyebabkan jari kaki melengkung, mengakibatkan kesakitan dan ketidakselesaan apabila berjalan atau memakai kasut. Jika tidak dirawat, keadaan ini boleh bertambah buruk, membawa kepada masalah kaki yang lebih teruk. Artikel ini akan membincangkan sebab, gejala, dan pilihan pengurusan untuk Sindrom Curly Toe di Singapura.
Menyebabkan
Sindrom Curly Toe adalah keadaan keturunan yang diturunkan dari ibu bapa kepada anak-anak mereka. Ia juga boleh disebabkan oleh keabnormalan dalam biomekanik kaki, seperti kaki rata. Keabnormalan dalam biomekanik kaki boleh menyebabkan ketidakseimbangan otot dan menyebabkan jari kaki melengkung atau bahkan mengembangkan kuku dan tukul.

Gejala-gejala
Gejala-gejala Sindrom Curly Toe boleh berbeza dari orang ke orang. Sesetengah orang mungkin tidak mempunyai gejala, sementara yang lain mengalami kesakitan dan ketidakselesaan yang teruk, terutamanya apabila memakai kasut yang ketat. Gejala biasa termasuk:
- Keriting jari kaki
- Kesakitan atau ketidakselesaan semasa berjalan atau memakai kasut
- Calluses atau jagung pada jari kaki yang terjejas
- Kemerahan atau bengkak di sekitar kaki yang terjejas
- Kuku jari kaki yang terjejas mungkin kelihatan rosak atau kelihatan seperti jangkitan kuku kulat
Pilihan Rawatan
Terdapat beberapa pilihan rawatan yang tersedia untuk Sindrom Curly Toe di Singapura. Walau bagaimanapun, pilihan rawatan terbaik untuk anda biasanya bergantung kepada keterukan keadaan anda dan keperluan individu anda. Pilihan rawatan standard termasuk:
- Latihan: Latihan flexion dan lanjutan jari kaki mudah boleh membantu meningkatkan kekuatan dan fleksibiliti jari kaki.
- Pelapik over-the-counter: Sesetengah pelindung kaki silikon yang tersedia secara komersial boleh membantu melegakan kesakitan dan ketidakselesaan buat sementara waktu.
- Orthotics: Insole yang dibuat khas boleh meningkatkan biomekanik kaki kita dan mengurangkan tekanan pada kaki yang terjejas.
- Pembedahan: Dalam kes-kes yang teruk di mana rawatan konservatif tidak berfungsi, pembedahan mungkin diperlukan untuk membetulkan kecacatan untuk mengurangkan kesakitan dan ketidakselesaan.
Pengurusan Kerinting Kaki di Singapura
Jika anda sedang mencari pilihan pengurusan untuk Sindrom Curly Toe di Singapura, kami sedia membantu. Pakar podiatrik kami yang berpengalaman dapat memberikan penilaian yang komprehensif dan rancangan pengurusan peribadi yang disesuaikan dengan keperluan anda. Kami juga menawarkan perkhidmatan anggota bawah yang lain, termasuk pengurusan sakit kaki dan buku lali , ortotik, dan penjagaan kaki diabetes. Hubungi kami hari ini untuk menjadualkan perundingan dan mengambil langkah pertama ke arah kaki yang lebih sihat dan bahagia.
Soalan lazim
Pihak pengurusan bergantung kepada keterukan keadaan. Ortotik, senaman kaki, dan kasut yang betul membantu untuk kes ringan hingga sederhana. Ortotik boleh membantu menyusun semula jari kaki dan postur kaki, manakala senaman kaki boleh membantu menguatkan otot dan meningkatkan fleksibiliti. Kasut yang betul juga boleh mengurangkan tekanan pada jari kaki dan mengelakkan kecacatan selanjutnya.
Sindrom jari kaki kerinting adalah kecacatan kaki yang agak biasa biasanya hadir semasa lahir. Ia boleh menjejaskan satu atau kedua-dua kaki dan lebih biasa dilihat pada wanita atau individu yang mempunyai sejarah keluarga.
Keadaan ini biasanya tidak hilang dengan sendirinya. Walau bagaimanapun, kita boleh menguruskan gejala dan mencegah keadaan daripada menjadi lebih teruk.
Kebanyakan kes sindrom jari kaki kerinting tidak memerlukan pembedahan. Walau bagaimanapun, pembedahan mungkin diperlukan untuk kes-kes yang lebih teruk, terutamanya apabila kecacatan itu tegar. Tujuan pembedahan dalam kes sedemikian adalah untuk membetulkan kecacatan dan melegakan kesakitan dan ketidakselesaan. Jika tidak, ortotik, latihan kaki, dan kasut yang betul boleh menguruskan kebanyakan kes.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Apabila mendiagnosis sakit kaki atau anggota bawah, ramai individu cenderung hanya memberi tumpuan kepada kawasan kesakitan. Oleh itu, kesan penjajaran badan terhadap kecederaan sering diabaikan. Sindrom Malalignment adalah keadaan biasa yang mempengaruhi bagaimana kaki anda berfungsi, menyebabkan kesakitan dan ketidakselesaan. Artikel ini akan menerangkan segala-galanya tentang keadaan ini, sebab dan gejala, dan cara menguruskannya.
Apakah Sindrom Malalignment?
Sindrom Malalignment adalah keadaan yang menjejaskan penjajaran badan anda, menyebabkan mereka berfungsi dengan tidak betul. Penjajaran badan yang lemah boleh membawa kepada pelbagai isu, termasuk kesakitan, ketidakselesaan, dan juga kecederaan. Sindrom Malalignment boleh berlaku disebabkan oleh beberapa faktor, termasuk genetik, sejarah kecederaan, dan penggunaan berlebihan. Kaki kita juga boleh menjejaskan postur keseluruhan kita, terutamanya jika seseorang mempunyai perbezaan kaki rata atau panjang kaki.
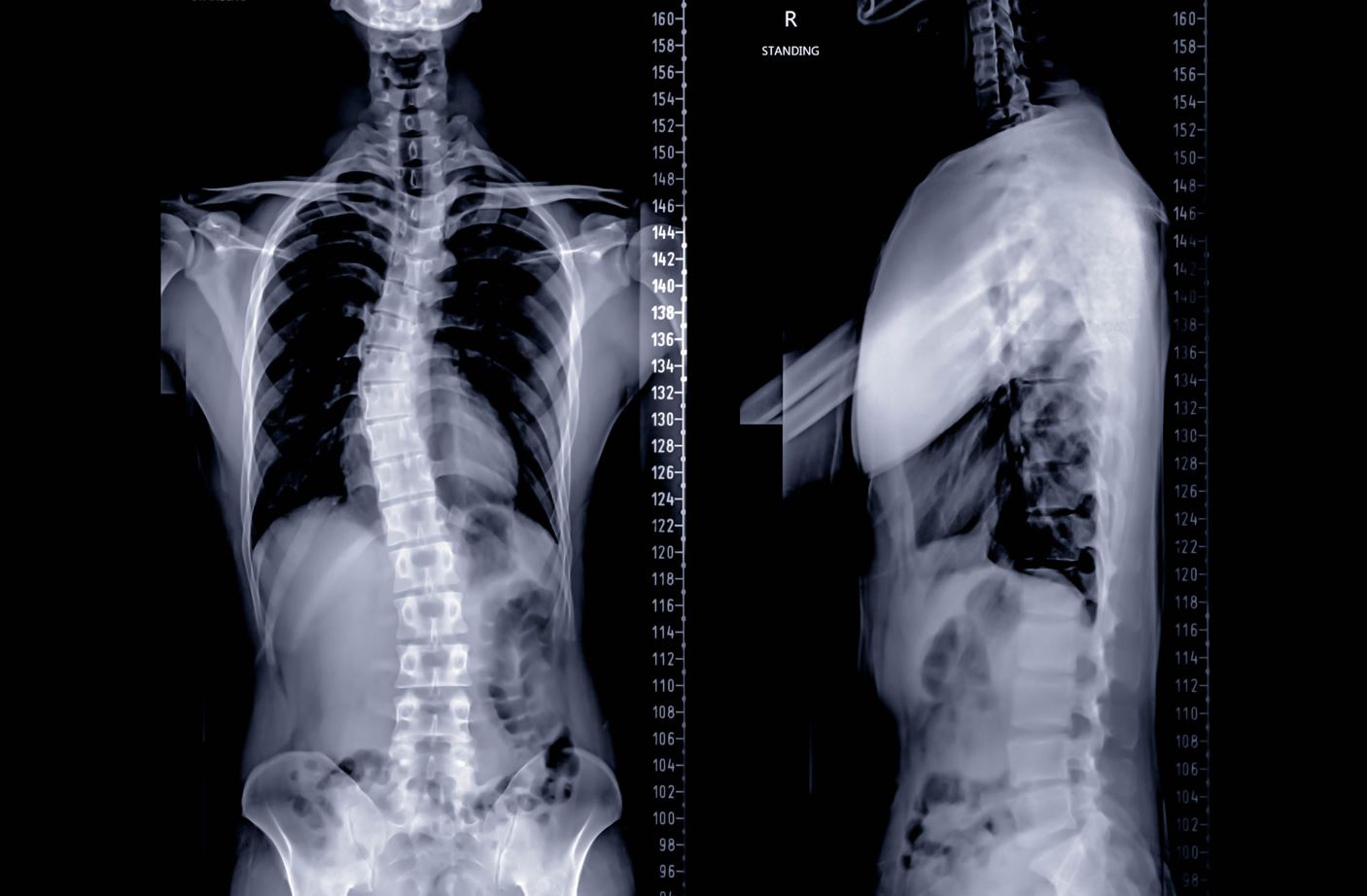
Gejala-gejala:
Gejala-gejala Sindrom Malalignment boleh berbeza-beza bergantung kepada keterukan keadaan. Gejala-gejala biasa termasuk:
- Sakit atau ketidakselesaan di kaki, pergelangan kaki, lutut, pinggul, atau bahagian bawah belakang
- Kesukaran berjalan atau berdiri untuk tempoh yang panjang
- Bengkak atau kelembutan di kawasan yang terjejas
- Ketegangan otot dan titik pencetus
- Pakai tidak sekata pada kasut

Punca Sindrom Malalignment:
Perubahan dalam penjajaran struktur kami boleh berlaku disebabkan oleh yang berikut:
- Genetik: Keadaan genetik seperti scoliosis atau kaki rata boleh menyebabkan postur yang lemah
- Kecederaan: Kecederaan pada kaki, buku lali, lutut, atau pinggul berpotensi menyebabkan penjajaran kita berubah
- Terlalu banyak digunakan: Penggunaan kaki yang berlebihan, terutamanya apabila seseorang mempunyai kedudukan yang lemah atau duduk postur
- Kasut yang lemah: Memakai kasut yang tidak sesuai dengan betul atau memberikan sokongan yang mencukupi boleh membuat perubahan dalam penjajaran anggota bawah
- Percanggahan panjang kaki: Panjang kaki yang tidak rata boleh menyebabkan penjajaran keseluruhan kami tidak berubah
Pengurusan untuk Sindrom Malalignment:
Di Straits Podiatry, kami menawarkan pelbagai pilihan pengurusan, termasuk:
- Ortotik tersuai: Ortotik tersuai ialah sisipan kasut yang direka khusus untuk membetulkan penjajaran kaki anda.
- Terapi fizikal: Terapi fizikal boleh membantu meningkatkan kekuatan, fleksibiliti, dan mobiliti di kawasan yang terjejas.
- Pelepasan titik pencetus: Melepaskan titik pencetus boleh melegakan ketegangan otot dan meningkatkan fleksibiliti otot
Kesimpulan:
Jika anda mengalami kesakitan atau ketidakselesaan di kaki, buku lali, atau lutut anda, adalah penting untuk mendapatkan rawatan perubatan. Di Straits Podiatry, kami pakar dalam menguruskan Sindrom Malalignment dan keadaan kaki yang lain. Pasukan podiatrik berpengalaman kami boleh membantu mendiagnosis dan menguruskan penyakit anda, membolehkan anda kembali ke aktiviti harian anda tanpa rasa sakit atau ketidakselesaan. Hubungi kami hari ini dan jadualkan temujanji!
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Di Straits Podiatry, kami percaya bahawa berjalan adalah bahagian penting dalam kehidupan dan memahami pentingnya berjalan dengan selesa dan bebas kesakitan. Kami pakar dalam menguruskan masalah kaki dan buku lali, termasuk berjalan kaki dan kaki luar pada kanak-kanak. Kami berhasrat untuk menyediakan penjagaan yang terbaik kepada pesakit kami di Singapura.
Kebimbangan umum ibu bapa tentang corak berjalan kaki anak-anak mereka adalah berjalan kaki dan kaki luar. Artikel ini akan membincangkan apa berjalan kaki dan kaki luar, bagaimana ia menjejaskan kaki dan kaki, dan pilihan pengurusan yang ada.
Berjalan kaki di kaki
Berjalan kaki kaki, juga dikenali sebagai berjalan kaki merpati, adalah di mana kaki berpusing ke dalam dan bukannya menunjuk lurus ke hadapan. Faktor genetik, kelemahan otot atau sesak, dan masalah perkembangan boleh menyebabkan keadaan ini.
Berjalan kaki boleh menyebabkan sakit kaki dan buku lali, terutamanya di jari kaki kecil dan kaki luar. Keadaan ini juga boleh menyebabkan terseliuh buku lali, sakit lutut, ketidakstabilan, dan kesukaran dengan keseimbangan dan koordinasi.

Berjalan kaki di luar
Berjalan kaki luar, juga dikenali sebagai kaki itik berjalan, adalah keadaan di mana kaki berpusing ke luar dan bukannya menunjuk lurus ke hadapan. Isu-isu seperti kaki rata, kelemahan otot atau ketat, dan perubahan dalam perkembangan tulang boleh menyebabkan keadaan ini.
Berjalan kaki di luar boleh menyebabkan sakit kaki dan buku lali, selalunya di pergelangan kaki dalam. Keadaan ini juga boleh menyebabkan sakit lutut, kaki letih, dan kesukaran dengan keseimbangan dan koordinasi.

Diagnosis dan Pengurusan
Di Straits Podiatry, kami akan menilai dengan teliti kaki dan kaki untuk mendiagnosis berjalan kaki dan keluar kaki. Kami menggunakan gabungan pemeriksaan fizikal dan analisis gaya berjalan untuk menentukan punca dan keterukan keadaan.
Pilihan pengurusan untuk berjalan kaki dan kaki luar mungkin termasuk ortotik tersuai, pendakap kaki pediatrik, terapi fizikal, regangan, dan latihan pengukuhan. Mendapatkan hasil yang positif memerlukan komitmen daripada ibu bapa dan anak-anak, jadi menjadikan pengurusan menyeronokkan untuk anak anda adalah penting.
Soalan yang kerap ditanya
Apakah In-toe atau Out-toe Gait?
In-toe dan out-toe berjalan merujuk kepada corak berjalan di mana kaki menunjuk ke dalam atau ke luar dan bukannya lurus ke hadapan. Corak berjalan ini biasanya diperhatikan pada kanak-kanak kecil dan kanak-kanak kecil dan boleh menyebabkan kebimbangan kepada ibu bapa. Berjalan kaki juga dipanggil berjalan kaki "merpati", manakala berjalan kaki di luar kadang-kadang dipanggil "berjalan itik."
Apa yang menyebabkan berjalan kaki luar?
Berjalan kaki di luar boleh mempunyai beberapa sebab yang mendasari, termasuk:
- Masalah pinggul: Dalam sesetengah kes, masalah pinggul boleh menyebabkan out-toeing. Keadaan pinggul seperti displasia pinggul boleh menjejaskan penjajaran kaki, yang membawa kepada corak berjalan.
- Masalah kaki: Sesetengah keadaan kaki, seperti metatarsus adductus atau kaki rata, boleh menyebabkan out-toeing.
- Cerebral palsy: Kanak-kanak cerebral palsy mungkin mengalami kesukaran mengawal otot kaki mereka, yang membawa kepada corak berjalan kaki atau kaki dalam.
Bilakah saya perlu bimbang tentang out-toeing?
Berjalan kaki biasanya bermula pada kanak-kanak kecil dan kanak-kanak kecil, tetapi penting untuk diperhatikan bahawa ia tidak selalu menjadi punca kebimbangan. Walau bagaimanapun, anda harus bercakap dengan podiatrist jika anda melihat mana-mana yang berikut:
- Kaki luar anak anda teruk, dan kaki mereka berpusing lebih daripada 30 darjah ke luar.
- Jari kaki anak anda semakin teruk dari semasa ke semasa.
- Anak anda mengalami kesakitan atau ketidakselesaan semasa berjalan atau berlari.
- Anak anda menunjukkan gejala lain, seperti limping atau berjalan kaki.
Mengapa In atau Out-toeing Bad?
Berjalan kaki dan kaki di luar boleh menjejaskan perkembangan kanak-kanak dalam beberapa cara. Sebagai contoh:
- In-toeing dan out-toeing boleh menjejaskan keseimbangan dan koordinasi kanak-kanak, yang membawa kepada jatuh dan kecederaan.
- In-toeing dan out-toeing boleh menyebabkan masalah pinggul dan lutut, yang membawa kepada kesakitan dan ketidakselesaan.
- In-toeing dan out-toeing boleh menjejaskan harga diri dan keyakinan kanak-kanak, terutamanya apabila mereka semakin tua.
Kesimpulan
Berjalan kaki dan berjalan kaki boleh membimbangkan ibu bapa, tetapi penting untuk memahami bahawa kita dapat menguruskan keadaan ini dengan diagnosis dan penjagaan yang betul. Di Straits Podiatry, kami komited untuk menyediakan penjagaan terbaik kepada anak anda di Singapura. Jadualkan janji temu dengan kami jika anda mempunyai kebimbangan tentang corak berjalan kaki anak anda.
Jika anda sedang mencari podiatrist yang dipercayai dan berpengalaman di Singapura, jangan cari lagi Straits Podiatry. Hubungi kami hari ini untuk menjadualkan temujanji anda dan mengambil langkah pertama ke arah berjalan kaki tanpa rasa sakit.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Sebagai podiatrists, kami memahami bahawa kaki kanak-kanak adalah penting untuk kesihatan dan kesejahteraan mereka secara keseluruhan. Oleh itu, artikel ini akan membincangkan keadaan muskuloskeletal yang paling biasa yang mempengaruhi kaki kanak-kanak dan bagaimana kita dapat menguruskannya.

Kaki Rata
Kaki rata, juga dikenali sebagai pes planus, adalah keadaan di mana terdapat kehilangan gerbang kaki. Keadaan ini biasa berlaku pada kanak-kanak dan biasanya pulih dengan sendirinya. Walau bagaimanapun, jika anak anda mengalami kesakitan atau ketidakselesaan, kami mengesyorkan anda mendapatkan bantuan profesional. Ortotik tersuai boleh ditetapkan untuk menyokong gerbang kaki dan mengurangkan kesakitan.
Penyakit Sever
Penyakit Sever adalah keadaan yang menjejaskan plat pertumbuhan di tulang tumit. Ia adalah keadaan biasa pada kanak-kanak aktif dan biasanya memberi kesan kepada mereka yang berumur antara 8 dan 14 tahun. Gejala termasuk sakit tumit, kelembutan, dan bengkak. Rehat, ais, dan kusyen tumit boleh membantu mengurangkan kesakitan, dan kami mengesyorkan mendapatkan bantuan profesional jika gejala berterusan.
Kuku jari kaki yang tumbuh
Kuku jari kaki berlaku apabila kuku tumbuh ke dalam kulit, menyebabkan kesakitan dan keradangan. Keadaan ini biasa berlaku pada kanak-kanak dan boleh disebabkan oleh kasut yang tidak sesuai atau pemangkasan kuku yang tidak betul. Kami mengesyorkan memakai kasut yang sesuai dengan baik dan mengelakkan stoking atau stoking yang ketat. Dalam kes-kes yang teruk, kita mungkin perlu mengeluarkan sebahagian atau semua kuku.
Ketuat Plantar
Ketuat plantar adalah jangkitan papillomavirus manusia (HPV) dan boleh menyakitkan dan hodoh. Keadaan ini biasa berlaku pada kanak-kanak dan boleh merebak melalui sentuhan dengan permukaan yang tercemar. Kami mengesyorkan anda mendapatkan bantuan profesional untuk menghilangkan ketuat, kerana rawatan di kaunter tidak berkesan.
SOALAN LAZIM
Apakah masalah kaki biasa dengan kanak-kanak?
Kaki kanak-kanak boleh mengalami pelbagai isu dan keadaan, termasuk kaki rata, ketuat plantar, kuku jari kaki, dan penyakit Sever. Keadaan ini boleh menyebabkan kesakitan, ketidakselesaan, dan mengehadkan mobiliti kanak-kanak. Diagnosis dan pengurusan yang betul adalah penting untuk mencegah komplikasi jangka panjang dan memastikan kaki anak anda kekal sihat.
Apakah kecacatan kaki pediatrik yang paling biasa?
Kecacatan kaki pediatrik yang paling biasa ialah kaki rata atau pes planus. Kaki rata berlaku apabila gerbang diratakan, menyebabkan kaki menyentuh tanah sepenuhnya. Walaupun ramai kanak-kanak akan mengatasi keadaan ini, yang lain mungkin mengalami kesakitan atau ketidakselesaan, dan ia mungkin memerlukan campur tangan profesional.
Apakah sakit kaki medial pada kanak-kanak?
Kesakitan kaki medikal pada kanak-kanak berlaku di bahagian dalam kaki, berhampiran gerbang. Pelbagai faktor, termasuk kaki rata, overpronation, dan kasut yang tidak betul, boleh menyebabkan sakit kaki tengah. Oleh itu, penilaian menyeluruh oleh podiatrist diperlukan untuk menentukan sebab asas dan membangunkan pelan pengurusan yang sesuai.
Apakah penilaian muskuloskeletal kaki?
Penilaian muskuloskeletal kaki adalah penilaian menyeluruh tulang, sendi, dan tisu lembut kaki dan buku lali. Penilaian ini dapat membantu mengenal pasti sebarang keadaan asas atau kecacatan yang mungkin memerlukan pengurusan dan juga dapat membantu mencegah masalah kaki masa depan. Podiatrist melakukan penilaian ini dan mungkin termasuk pelbagai ujian gerakan, analisis gaya berjalan, dan kajian pengimejan.
Kesimpulan
Di Straits Podiatry, kami memahami kepentingan kaki yang sihat pada kanak-kanak. Jika anak anda mengalami sebarang sakit kaki atau buku lali, kami sangat mengesyorkan mendapatkan bantuan profesional. Pasukan podiatrik berpengalaman kami dapat memberikan penilaian dan pengurusan yang komprehensif untuk memastikan kaki anak anda sihat dan bebas kesakitan. Hubungi kami hari ini untuk menjadualkan temujanji.
Dengan memberikan maklumat yang komprehensif mengenai keadaan muskuloskeletal biasa yang mempengaruhi kaki kanak-kanak, kami berhasrat untuk mendidik ibu bapa dan penjaga tentang pentingnya mendapatkan bantuan profesional apabila perlu. Pasukan kami di Straits Podiatry berdedikasi untuk menyediakan penjagaan berkualiti tinggi dan memastikan kaki anak anda kekal sihat dan bebas daripada kesakitan.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Jika anak anda mengalami kesakitan yang semakin meningkat, adalah penting untuk memahami apa yang mereka ada, apa yang menyebabkan mereka, dan bagaimana untuk menguruskannya. Sebagai satu pasukan pakar podiatri di Singapura, kami memahami bagaimana kesakitan ini boleh menjadi punca kebimbangan kepada ibu bapa. Artikel ini akan merangkumi semua yang anda perlu tahu tentang kesakitan yang semakin meningkat, termasuk gejala, sebab, dan pilihan rawatan.
Memahami Kesakitan Yang Semakin Meningkat
Kesakitan yang semakin meningkat adalah aduan kanak-kanak biasa yang biasanya berlaku di kaki. Mereka sering berlaku pada lewat petang atau petang dan berlangsung beberapa jam. Pada masa yang sama, mereka boleh menjadi sangat tidak selesa. Mereka biasanya tidak menjadi punca kebimbangan dan tidak menyebabkan kerosakan jangka panjang.

Apakah Simptom-simptomnya?
Kesakitan yang semakin meningkat biasanya menyebabkan sensasi sakit atau berdenyut di kaki. Kesakitan biasanya berlaku di bahagian depan paha, betis, atau di belakang lutut. Beberapa gejala biasa yang lain juga termasuk:
- Keletihan atau keletihan
- Kegelisahan atau kesukaran tidur
- Kerengsaan atau perubahan mood
Apa yang menyebabkan kesakitan?
Punca sebenar kesakitan yang semakin meningkat tidak diketahui. Walau bagaimanapun, terdapat beberapa teori tentang apa yang boleh menyumbang kepada kejadian mereka, dan mereka termasuk yang berikut:
- Lonjakan pertumbuhan pesat
- Keletihan otot daripada peningkatan aktiviti
- Postur yang lemah atau mekanik kaki
- Genetik
Bagaimana untuk merawat kesakitan?
Walaupun tiada ubat khusus untuk sakit yang semakin meningkat, beberapa pilihan rawatan boleh membantu menguruskan gejala. Beberapa pilihan rawatan yang paling berkesan termasuk:
- Mengurut kawasan yang terjejas
- Memohon pek haba atau sejuk
- Latihan regangan
- Ubat sakit tanpa preskripsi, seperti ibuprofen atau acetaminophen
Sebagai tambahan kepada pilihan rawatan ini, memastikan anak anda mendapat tidur yang cukup, makan diet yang sihat, dan terlibat dalam aktiviti fizikal yang kerap adalah penting. Jika gejala anak anda berterusan atau menjadi lebih teruk, adalah penting untuk mendapatkan nasihat perubatan.

Bagaimanakah Podiatry boleh membantu?
Sebagai pakar podiatri, kami memahami bahawa sakit yang semakin meningkat kadang-kadang boleh menjadi gejala keadaan kaki atau buku lali yang mendasari. Sebagai contoh, kaki rata atau gerbang tinggi boleh menyebabkan keletihan otot dan membawa kepada gejala yang sama. Jika anda bimbang tentang kesakitan anak anda, menjadualkan temujanji dengan podiatrist adalah penting.
Pasukan podiatrik berpengalaman kami boleh memeriksa dengan teliti untuk menentukan sama ada sebarang keadaan kaki atau buku lali yang mendasari boleh menyumbang kepada gejala anak anda.
Pada usia berapa anda mendapat kesakitan yang semakin meningkat?
Kesakitan yang semakin meningkat biasanya berlaku pada kanak-kanak berumur antara 3 dan 12 tahun, dengan kebanyakan kes melibatkan kanak-kanak berumur antara 4 dan 8 tahun. Adalah luar biasa bagi remaja dan orang dewasa untuk mengalami keadaan ini kerana ia biasanya mereda apabila kanak-kanak berumur.
Berapa lama kesakitan yang semakin meningkat boleh bertahan?
Ia biasanya ringkas, dengan kebanyakan episod berlangsung selama 10 hingga 30 minit pada satu masa. Kesakitan sering berlaku, dengan sesetengah kanak-kanak mengalami suar beberapa kali seminggu. Walau bagaimanapun, kesakitan biasanya berselang-seli dan tidak tetap. Keadaan ini boleh berterusan selama beberapa bulan atau tahun tetapi secara amnya, selesaikan pada masa kanak-kanak mencapai masa remaja.
Apa yang boleh disalah anggap sebagai sakit yang semakin meningkat?
Kesakitan yang semakin meningkat boleh disalah anggap sebagai keadaan lain, seperti patah tulang, jangkitan, gangguan reumatik, atau keadaan perubatan asas yang lain. Adalah penting untuk berunding dengan podiatrist jika anak anda mengalami kesakitan yang berterusan atau teruk dengan bengkak atau kemerahan. Podiatrist boleh memeriksa dengan teliti dan menolak sebarang kemungkinan penyebab kesakitan yang lain.
Adakah kesakitan yang semakin meningkat adalah perkara sebenar?
Ya, kesakitan yang semakin meningkat adalah keadaan perubatan sebenar. Kesakitan biasanya berlaku di kaki, terutamanya di paha, betis, dan di belakang lutut. Walaupun punca sebenar tidak difahami sepenuhnya, ia dipercayai berkaitan dengan pertumbuhan normal kanak-kanak dan perkembangan tulang dan otot.
Bagaimana kesakitan yang semakin meningkat bermula?
Kesakitan yang semakin meningkat biasanya bermula pada waktu petang atau pada waktu malam dan boleh membangunkan kanak-kanak itu. Kesakitan sering digambarkan sebagai sakit atau berdenyut dan boleh berlaku dalam satu atau kedua-dua kaki. Kesakitan juga boleh berbeza-beza dalam intensiti, dengan sesetengah kanak-kanak mengalami ketidakselesaan ringan manakala yang lain mungkin mengalami kesakitan yang lebih teruk. Mengurut kawasan yang terjejas, regangan, atau memohon haba secara amnya membantu melegakan kesakitan.
Betapa menyakitkannya kesakitan yang semakin meningkat?
Kesakitan yang semakin meningkat boleh menyakitkan bagi sesetengah kanak-kanak tetapi biasanya tidak teruk. Kesakitan sering sakit atau berdenyut, dari intensiti ringan hingga sederhana. Kesakitan biasanya berselang-seli dan tidak tetap. Kebanyakan kanak-kanak boleh meneruskan aktiviti normal mereka sebaik sahaja rasa sakit berkurangan. Sekiranya kesakitan itu teruk atau berterusan, berunding dengan podiatrist untuk penilaian dan rawatan lanjut adalah penting.
Kesimpulan
Kesakitan yang semakin meningkat adalah aduan kanak-kanak biasa yang boleh menjadi tidak selesa dan membimbangkan ibu bapa. Sebagai pakar podiatri, kita faham ini kadang-kadang boleh menjadi gejala keadaan kaki atau buku lali yang mendasari. Walaupun tiada penawar khusus wujud, beberapa pilihan rawatan boleh membantu menguruskan gejala. Jika anda bimbang tentang kesakitan anak anda yang semakin meningkat, menjadualkan temujanji dengan podiatrist adalah penting. Pasukan podiatrik berpengalaman kami boleh melakukan pemeriksaan menyeluruh dan memberi anda pilihan rawatan terbaik untuk membantu menguruskan kesakitan anak anda.
Jika anda berada di Singapura yang mencari klinik podiatri, kami menjemput anda untuk melawat Straits Podiatry. Pasukan podiatrik berpengalaman kami boleh memberikan penjagaan terbaik untuk semua keperluan kaki dan buku lali anda. Hubungi kami hari ini untuk menjadualkan temujanji.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
As parents, we are always concerned about our children’s health. One of the common foot conditions that affect children is ingrown toenails. It can cause discomfort, pain, and sometimes lead to infection if left untreated. In this article, we will discuss the causes, symptoms, and the best solutions available for ingrown toenails in children in Singapore to help you and your child get relief from this condition.
What are Ingrown Toenails?
Ingrown toenails in children occur when the edge of the toenail grows into the surrounding skin, causing pain and discomfort. It can affect any toe, but it is more common in the big toe. Ingrown toenails can be caused by a variety of factors, such as improper nail trimming by parents, wearing tight shoes, or injury to the toe.

Causes of Ingrown Toenails in Children
Ingrown toenails in children can be caused by several factors, including:
- Poor nail trimming techniques: Cutting the toenail too short or rounding the edges can cause the nail to grow into the surrounding skin.
- Tight-fitting shoes: Wearing shoes that are too small or narrow can put pressure on the toenails and cause them to grow into the skin. Learn how to select the right shoe for you.
- Injury to the toe: Stubbing the toe or dropping a heavy object on it can cause the nail to grow into the skin.
Symptoms of Ingrown Toenails
The most common symptom of an ingrown toenail in children is pain and discomfort. Other symptoms include:
- Redness and swelling around the affected nail
- Tenderness to touch
- Pus or discharge around the nail
- Difficulty walking or wearing shoes
Management of Ingrown Toenails in Children
There are several treatments available in Singapore. The treatment options depend on the severity of the condition.
- Soak the affected foot in warm water: Soaking the foot in warm water for 15-20 minutes, 2-3 times a day, can help reduce pain and swelling.
- Nail trimming: Your podiatrist may trim the nail spike to provide immediate pain relief.
- Antibiotics: If the ingrown toenail is infected, your podiatrist may refer you to see a GP for antibiotics after the nail spike is removed.
- Surgical Treatment: This is rarely performed for children with ingrown toenails and is only conducted if the condition is very severe.
Kesimpulan
Ingrown toenails in children can cause pain and discomfort if left untreated. It is important to seek medical attention if your child experiences any symptoms of an ingrown toenail. At Straits Podiatry in Singapore, our experienced podiatrists specialize in the management of foot and ankle conditions, including ingrown toenails. Contact us today to schedule an appointment and let us help your child get relief from this condition.
Patients Also Asked
1. How do you treat an ingrown toenail in a child?
To treat an ingrown toenail on a child, there are several steps you can take. First, you should soak your child’s foot in warm water for 15-20 minutes, three to four times a day. This can help to reduce swelling and ease pain. You can also gently separate the edge of the ingrown toenail and the skin with a clean, sterile piece of cotton under it. This can help to lift the nail away from the skin and relieve pressure. If the pain persists, bring your child to see a podiatrist. If the ingrown toenail is infected, your child may need antibiotics.
2. Is it normal for kids to get ingrown toenails?
Yes, it is normal for kids to get ingrown toenails. This is because their toenails are very thin and sharp, they can also easily become misshapen or curved. Ingrown toenails in children can also be caused by tight shoes or socks, poor nail care, and injuries to the toenail. If your child has an ingrown toenail, it is important to address it as soon as possible to prevent infection and further complications.
3. When should I take my child to the podiatrist for an ingrown toenail?
If your child has an ingrown toenail and experiences severe pain, redness, swelling, or pus, you should take them to the podiatrist as soon as possible. These symptoms may indicate an infection that requires medical attention. Additionally, if your child has diabetes or other medical conditions that affect circulation or immune function, you should seek medical advice immediately.
4. Can a 7-year-old get an ingrown toenail?
Yes, a 7-year-old can get an ingrown toenail. Children of any age can develop this condition. However, it is more common in older children and teenagers who are more likely to wear tight shoes and engage in activities that can cause injury to the toenail.
5. How do you fix an ingrown toenail on a 5-year-old?
To fix an ingrown toenail on a 5-year-old, you should follow the same steps as for older children. Start by soaking the affected foot in warm water. You can then place a small piece of sterile cotton at the side of the nail to relieve pressure. If the toenail is infected or your child experiences severe pain, you should seek medical advice from a podiatrist.
6. What is the fastest way to fix an ingrown toenail in children?
There is no one-size-fits-all answer to this question, as the treatment depends on the severity of the condition. However, soaking the affected foot in warm water several times a day and gently lifting the edge of the nail can help to relieve pain and pressure. If the toenail is infected or your child experiences severe pain, you should seek medical advice. Your child’s podiatrist may prescribe antibiotics or recommend a minor surgical procedure to remove the ingrown portion of the nail.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
We understand that dealing with paronychia can be a painful and frustrating experience. Hence, we’ve put together this comprehensive guide to help you understand what paronychia is, what causes it, and how to manage it effectively.
What is Paronychia?
Paronychia is an infection of the skin around a fingernail or toenail. It can be acute or chronic and can affect anyone, regardless of age or gender. Its symptoms can vary, but they usually include redness, swelling, pain, and tenderness around the affected nail. In some cases, pus may also develop. Paronychia often occurs together with an ingrown toenail, however, it is important to differentiate them.

What Causes Paronychia?
Paronychia is typically caused by bacteria or fungi entering the skin around the nail. The infection can occur due to a break in the skin, such as a cut or hangnail, or as a result of damage caused by manicures or pedicures. Certain medical conditions, such as diabetes, can also increase the risk of developing this condition.
How is Paronychia Treated?
Treatment for paronychia depends on the severity of the infection. In mild cases, soaking the affected area in warm water several times a day can help reduce swelling and promote healing. Antiseptic creams or ointments may also be recommended. In moderate cases, oral antibiotics may be necessary. In severe cases, drainage or removal of the nail may be required.
Can Paronychia be Prevented?
There are several steps you can take to reduce your risk of developing paronychia. These include:
- Keeping your hands and feet clean and dry
- Avoiding biting or picking at your nails
- Avoiding harsh chemicals and soaps that can dry out the skin around your nails
- Keeping your nails trimmed and filed to prevent hangnails and other types of nail trauma
What is the main cause of paronychia?
Paronychia is a common nail infection that occurs when bacteria or fungi enter the skin around the nail. It is most commonly a bacterial infection, typically caused by Staphylococcus aureus. However, fungal infection can also occur, especially in people who frequently expose their nails to water or have weakened immune systems.
What is the fastest way to get rid of paronychia?
The fastest way to get rid of paronychia is to seek medical treatment. Your doctor may prescribe antibiotics to treat the infection or may drain any pus that has accumulated. You can also take steps at home to help reduce symptoms, such as soaking the affected finger or toe in warm water for 15-20 minutes several times a day and keeping the area clean and dry.
What does paronychia look like?
Paronychia can cause redness, swelling, and tenderness around the affected nail. The area may also feel warm and may be filled with pus. In some cases, the skin around the nail may peel or become thickened. In chronic cases, the skin may become discoloured and the nail may become distorted or misshapen.

What is the best treatment for paronychia?
The best treatment for paronychia depends on the severity of the infection. In mild cases, home remedies such as warm water soaks and keeping the area clean and dry may be sufficient. In more severe cases, your doctor may also prescribe antibiotics or drain any pus that has accumulated. It is important to seek medical treatment if the infection appears to be spreading or if you have a fever or other symptoms.
Can I ignore paronychia?
It is not recommended to ignore paronychia as it can lead to more serious infections if left untreated. In addition, it can cause permanent damage to the nail and surrounding tissues. It is important to seek medical treatment if you suspect you have this condition, especially if you have a weakened immune system or if the infection appears to be spreading.
Does salt water help paronychia?
Soaking the affected finger or toe in warm salt water can help to relieve pain and reduce inflammation associated with paronychia. However, it is important to note that this remedy should not be used as a substitute for medical treatment. If you suspect you have paronychia, it is important to seek medical treatment to prevent the infection from spreading or becoming more severe.
Kesimpulan
At Straits Podiatry, we understand how frustrating it can be to deal with paronychia. If you’re experiencing symptoms, we encourage you to seek relief as soon as possible. Our experienced podiatrists can provide you with a comprehensive evaluation and develop a personalized management plan to help you get back to your normal routine as quickly as possible. Don’t let the pain hold you back – contact us today to schedule your appointment.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
At Straits Podiatry, we understand that postural issues in children can be a concerning matter for parents. Poor postural habits can lead to a wide range of musculoskeletal problems in the future, making it essential to address them early on. In this article, we’ll take a closer look at common postural issues in children and explore how podiatry can help address these problems.

Understanding Postural Issues in Children
Posture refers to the alignment of the body’s joints and muscles while standing, sitting, or lying down. When a child has poor posture, it means that their body is not aligned correctly. This can cause potential strain on their muscles, bones, and ligaments. In the long term, poor posture can cause chronic pain and even structural malalignment.
Common postural issues in children include:
Kaki Rata
Flat feet are a common postural issue in children, where the arch of the foot collapses, causing the entire foot to make contact with the ground. This lead to overpronation (inward rolling of the feet) and can cause issues such as ankle pain, knee pain, and lower back pain.
Lutut Ketukan
Knock knees occur when a child’s knees come together while standing, while their ankles remain apart. This condition can cause an imbalance in the body’s alignment, leading to potential issues in the feet, hips, and spine.
Berjalan Kaki
Toe walking is a habit where a child walks on their toes, without their heels touching the ground. While toe walking is not always a problem, it can cause problems if the child does it long-term. Toe walking causes issues with the calf muscles, Achilles tendon, and even leads to balance issues.
Percanggahan Panjang Kaki
Leg length discrepancy is a condition where one leg is longer than the other. The difference in leg length can cause uneven hips and potentially scoliosis of the spine.

What are postural disorders in children?
Postural disorders are conditions that affect a child’s posture while standing, sitting, or lying down. These conditions can affect the alignment of the joints and muscles and can lead to chronic pain and discomfort if left untreated.
What causes poor posture in children?
There are a variety of factors that can cause poor posture in children, including:
- Spending too much time in sedentary activities, such as watching TV or playing video games
- Carrying heavy backpacks or school bags
- Poorly designed furniture, such as non-ergonomically designed desks and chairs
- Certain medical conditions, such as scoliosis or cerebral palsy
What are the 3 common posture problems?
The three most common posture problems in children are:
- Flat Feet – where the arch of the foot collapses, causing the entire foot to make contact with the ground.
- Knock Knees – where a child’s knees come together while standing, while their ankles remain apart.
- Toe Walking – where a child walks on their toes, without their heels touching the ground.
- Leg Length Discrepancy – where a child has a longer leg on one side.
What are the 4 types of postural disorder?
There are four main types of postural disorders that can affect children:
- Kyphosis – This is a condition where the upper back is excessively curved in a “hunchback” appearance. Poor posture, spinal injuries, or developmental problems can cause kyphosis.
- Lordosis: This is a condition where the lower back is excessively curved, causing the abdomen and buttocks to stick out. Lordosis can be caused by poor posture, obesity, or muscular imbalances.
- Scoliosis: This is a condition where the spine is curved to the side, resulting in an “S” or “C” shape. Scoliosis can be caused by developmental problems, spinal injuries, or genetic factors.
- Flat Feet: This is a condition where the arches of the feet are collapsed, causing the entire foot to touch the ground. Flat feet can be caused by genetic factors, muscular imbalances, or excessive weight-bearing activities.
Bagaimanakah Podiatry boleh membantu?
Podiatrist can help to address postural disorders in children when the underlying cause is arising from the lower limb. This includes an assessment of flat feet, leg length discrepancy, and your child’s gait pattern.
Treatment options are usually dependent on the underlying cause but can include:
- Ortos kaki tersuai
- Supramalleolar orthoses
- Knee braces
- Exercises and rehabilitation
At Straits Podiatry, we offer a range of management options that can help address postural issues in children. Our team of experienced podiatrists can assess your child’s posture, gait, and foot structure, and recommend appropriate solutions.
Kesimpulan
Postural issues in children can be a concern for parents, but they can be effectively addressed with the right management. At Straits Podiatry, our team of experienced podiatrists can help assess your child’s posture and recommend appropriate management. Contact us today to schedule an appointment and take the first step towards better postural health for your child.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Arthritis is a common condition that affects millions of people globally, and it can cause significant pain and discomfort in the foot and ankle joints. If you are based in Singapore and experiencing symptoms of arthritis, such as joint pain, stiffness, and swelling, it is essential to seek medical attention from a qualified healthcare provider. In this article, we will share some advice for foot and ankle arthritis management in Singapore.
Types of Foot and Ankle Arthritis
Different types of arthritis can affect the foot and ankle, including osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis. Osteoarthritis is often seen in older adults and is caused by the wear and tear of the joint over time. Rheumatoid arthritis is an autoimmune disorder that can affect any joint in the body, including those in the foot and ankle. After a foot or ankle injury, post-traumatic arthritis can develop.

How to Treat Foot and Ankle Arthritis?
If you’re in Singapore and experiencing arthritis symptoms, seek help from a local healthcare provider. They can diagnose the type of arthritis you have and provide treatment options that may include medications, physical therapy, or surgery.
In addition to seeking medical attention, you can also take steps at home to manage your arthritis symptoms. Some short-term steps include resting the affected joint, applying ice to reduce swelling, and taking over-the-counter pain medications. However, for longer-lasting improvements, you should do exercises to improve flexibility and strength, wear supportive shoes that fit well, and use orthotics or other devices to support the affected joint.
Don’t Let Joint Pain Limit Your Activities
Remember, managing arthritis is crucial to improving your quality of life. Don’t let joint pain or discomfort keep you from enjoying daily activities. Seek help from a healthcare provider and take steps at home to manage your symptoms.
It’s also important to note that managing arthritis requires a long-term approach. While treatment options can help manage symptoms, they may not cure the condition. Therefore, it’s crucial to maintain a healthy lifestyle to help reduce the impact of arthritis on your daily life. Things you can start doing are regular exercise and a balanced diet. Always remember that the joint will be more painful and stiff if you keep resting.
Foot and Ankle Arthritis Treatment in Singapore
In Singapore, several healthcare providers specialize in treating arthritis and other foot and ankle conditions. At Straits Podiatry, we are able to help manage arthritis along side other medical professionals. Our team of experienced podiatrists offer personalized management plans to address a wide range of foot and ankle issues, including arthritis.
At Straits Podiatry, our team uses the latest technology and techniques to provide their patients with effective and efficient management options. Our services include custom orthotics, shockwave therapy, and magnetotransduction therapy. These can help manage arthritis symptoms and improve overall foot health.
If you’re in Singapore and experiencing symptoms of arthritis or other foot conditions, look no further. Do not hesitate to schedule an appointment with Straits Podiatry. Our team of podiatrists can help diagnose the issue and provide personalized management options to help manage your symptoms and improve your quality of life.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
At our podiatry clinic in Singapore, we understand how debilitating foot pain can be. One of the most common causes of foot pain is a Plantar Plate Tear or Plantar Plate Injury. Pain from the plantar plate is usually quite distinct as it normally feels like you are stepping on a pebble. In this article, we will discuss the causes, symptoms, diagnosis, and management options for this condition.
What is a Plantar Plate Tear?
The plantar plate is a ligament located under the ball of the foot, connecting the toes to the metatarsal bones. A tear occurs when this ligament is degenerated or suffered too much trauma, leading to pain and discomfort in the ball of the foot. This condition is common among athletes, especially those who engage in high-impact sports like running and jumping.
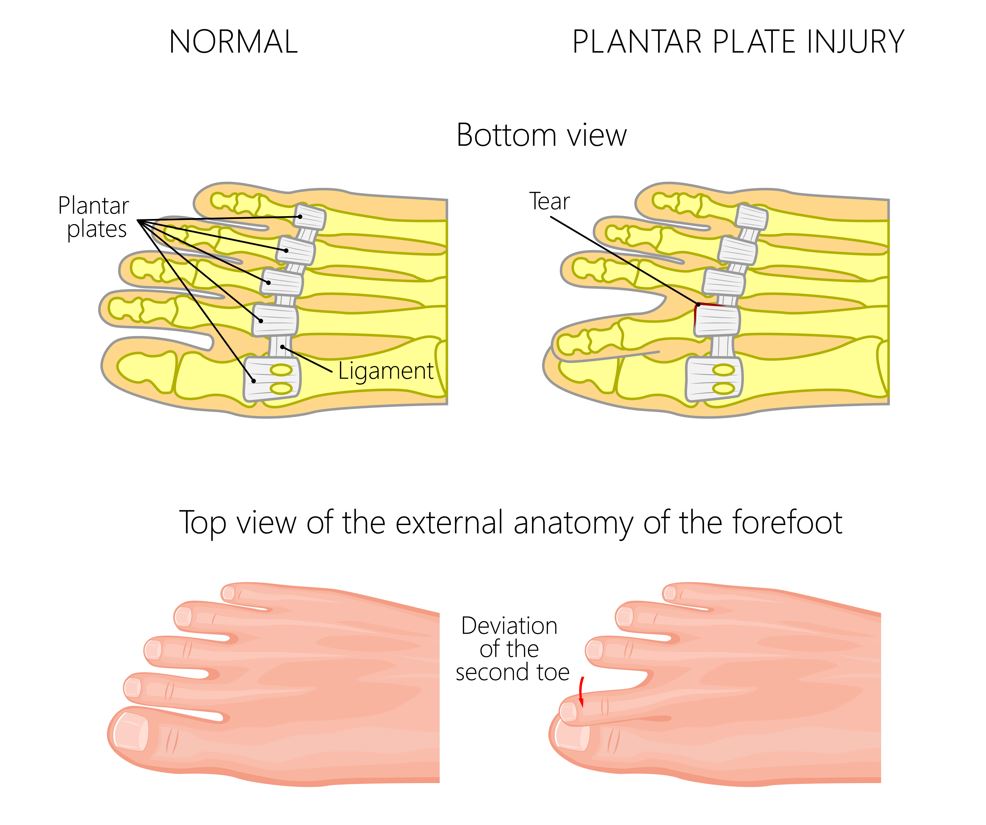
Causes of Plantar Plate Tear
There are several factors that can contribute to the development of this condition. Some of the most common causes are:
- Overuse: Engaging in repetitive high-impact activities can cause stress on the plantar plate, leading to tears over time.
- Foot Structure: People with high arches or flat feet are more prone to developing plantar plate injuries.
- Trauma: A direct injury to the ball of the foot, such as stubbing the toe, can cause the tear to occur
Symptoms of Plantar Plate Tear
The most common symptom is pain in the ball of the foot, especially when walking or standing. Patients will usually describe plantar plate pain as “stepping on a pebble”. Other symptoms may include:
- Bengkak
- Kemerahan
- Tenderness
- Kekakuan
- Retracted toe (“floating toe”)
Plantar Plate Tear Diagnosis
A podiatrist can diagnose a plantar plate tear by performing a physical examination and taking a medical history. Imaging tests like diagnostic ultrasound and MRIs may also be used to confirm the diagnosis and determine the extent of the injury.
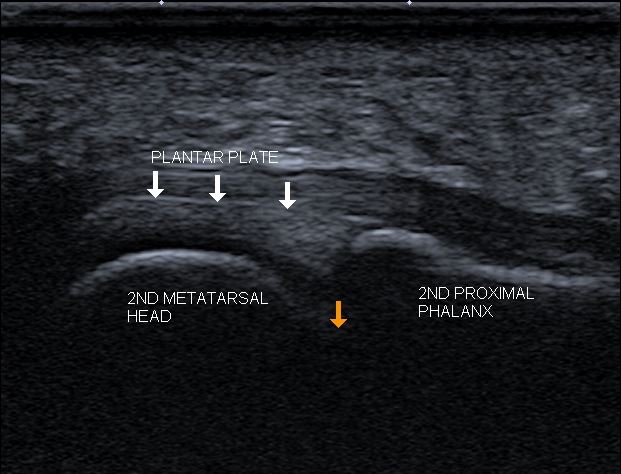
Treatment for plantar plate pain typically involves a combination of rest, physical therapy, and medication. In some cases, surgery may be necessary to repair the tear.
Treatment Options for Plantar Plate Tear
- Rest: Resting the foot and avoiding high-impact activities can help reduce pain and inflammation.
- Orthotics: Podiatrist-prescribed customised insoles can be designed to specifically take pressure off the affected toe joint and reduce pain
- Advanced Therapies: Management options such as shockwave therapy and magnetotransduction therapy can help to stimulate repair, and reduce pain and inflammation.
- Medication: Over-the-counter pain relievers like ibuprofen, though not recommended, can help reduce pain and inflammation.
- Surgery: If conservative treatments do not provide good relief, surgery may be necessary to repair the tear.
Kesimpulan
Plantar plate tears can be a painful and debilitating condition, but with proper diagnosis and management, patients can recover and return to their normal activities. If you are experiencing foot pain or suspect you may have a plantar plate injury, contact our podiatry clinic in Singapore today to schedule an appointment with one of our experienced podiatrists. Let us help you get back on your feet!
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Peroneal tendonitis is a common foot and ankle condition that can cause pain, inflammation, and swelling at the outer ankle. It occurs when the peroneal tendons, which are responsible for stabilizing the ankle and foot, become inflamed or damaged. In this article, we will discuss the symptoms, causes, and treatment options for peroneal tendonitis in Singapore, as well as ways to prevent it.
Gejala-gejala
The symptoms of peroneal tendonitis can vary based on the severity of the condition. Yet, the following are some of the most common symptoms:
- Ankle pain on the outside of the ankle
- Swelling in the affected area
- Stiffness in the ankle and foot
- Weakness in the ankle and foot
- Instability or trouble walking
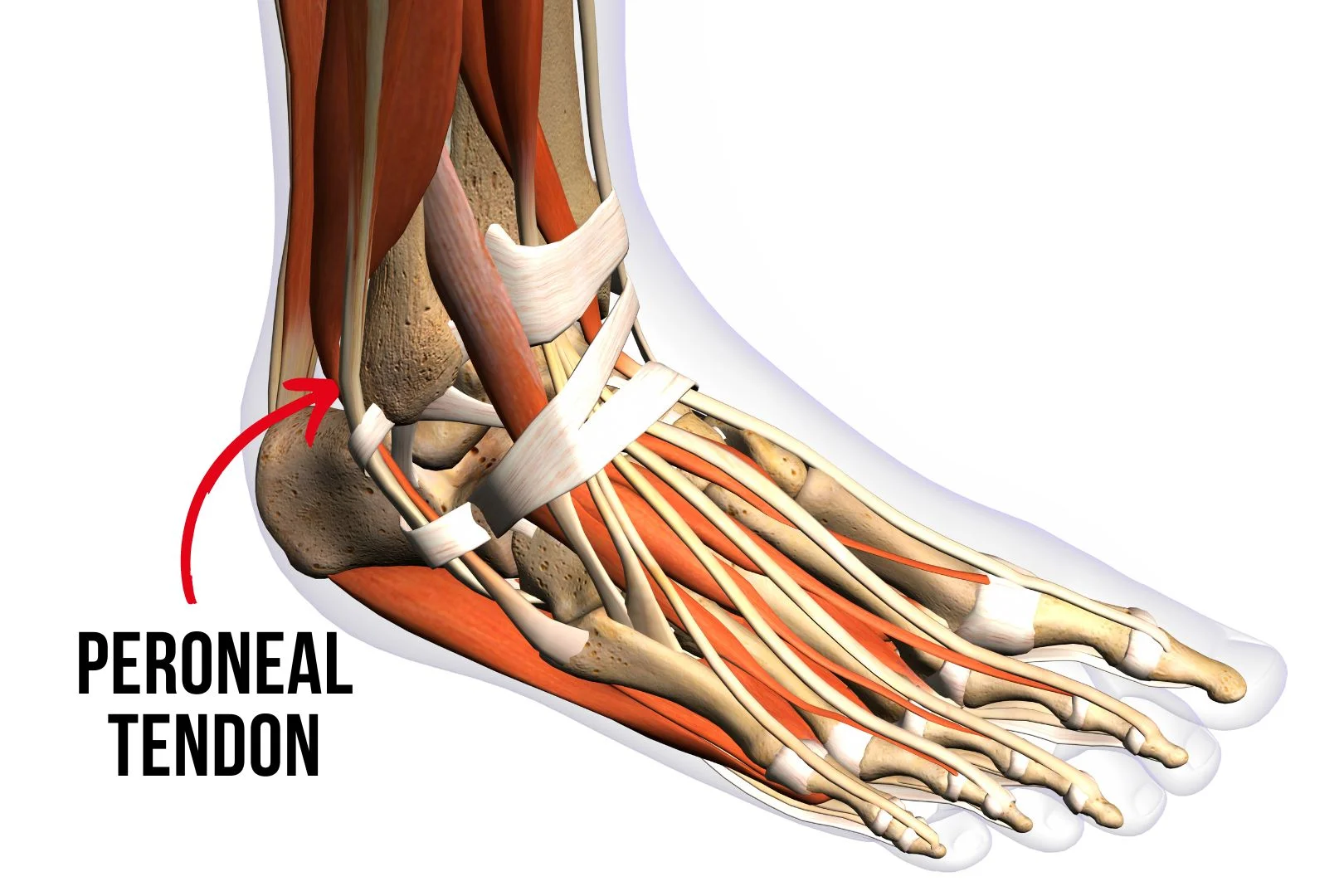
Menyebabkan
Peroneal tendonitis can be caused by a variety of factors, including:
- Overuse or repetitive strain on the peroneal tendons
- Ankle sprains or other injuries that damage the tendons
- Poor foot mechanics or foot structure
- Kaki rata
- Wearing improper footwear
- Tight or weak muscles in the lower leg and foot
Peroneal Tendonitis Treatment Options in Singapore
There are several treatment options for peroneal tendonitis in Singapore, including:
- Rest and ice: Resting the affected area and applying ice can help reduce pain and swelling.
- Physical therapy: Stretching and strengthening exercises can help improve the flexibility and strength of the ankle and foot.
- Orthotics: Wearing custom-made insoles in your shoes can help support the foot and reduce strain on the peroneal tendons.
- Shockwave therapy: Focused shockwave therapy can help to reduce pain, and inflammation, and stimulate more blood flow to heal the tendon
- Medications: Although not advisable to take, over-the-counter pain medicines, such as ibuprofen, can help reduce pain and inflammation.
- Surgery: In very severe cases, surgery may be necessary to repair the damaged tendons.
Pencegahan
To prevent peroneal tendonitis, it is important to:
- Wear proper shoes that provide support and cushioning for the foot
- Gradually increase the intensity and duration of physical activity
- Stretch and strengthen the muscles in the lower leg and foot
- Use insoles or inserts to support the foot and reduce strain on the tendons
- Seek prompt medical attention for any ankle or foot injuries
Kesimpulan
Peroneal tendonitis can be painful and uncomfortable, but it can be managed with the right care and management. If you are experiencing symptoms of peroneal tendonitis, it is important to seek prompt medical attention to prevent further damage and problems. At Straits Podiatry, our team of expert podiatrists can provide you with the right treatment options for peroneal tendonitis and other foot and ankle conditions. Contact us today to schedule an appointment and get on the path to a healthy life without pain.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Flat feet, also known as fallen arches, is a condition where the arch of the foot collapses, causing the entire foot to make contact with the ground. Flat feet in Singapore is extremely common and it affects millions of people around the world. In this article, we will discuss the causes, symptoms, and treatment options for flat feet in Singapore.
Apakah Kaki Rata?
Flat feet, also known as pes planus, is a common condition where the arches of the feet are lower than normal or non-existent. This can lead to the entire foot making contact with the ground when standing or walking.

Causes of Flat Feet in Singapore
Flat feet can be caused by a variety of factors, including:
- Genetics: if flat feet run in your family, you may be more likely to develop the condition
- Injury: a foot or ankle injury can cause the arch to collapse, such as posterior tibial tendon dysfunction or Lisfranc injury
- Age: as we age, the tendons and ligaments in our feet can weaken, leading to flat feet
- Obesity: being overweight can put extra pressure on the feet, leading to flat feet
- Pregnancy: the extra weight and pressure on the feet, as well as hormonal changes during pregnancy, can cause the arch to collapse
Symptoms of Flat Feet in Singapore
Some people with flat feet may not experience any symptoms. However, others may experience:
- Pain in the feet, ankles, or legs, especially after standing or walking for long periods of time
- Swelling along the inside or outside of the ankle
- Difficulty standing on tiptoe
- Flat shoes that wear out quickly on the inside of the sole
- Foot or leg fatigue
Diagnosis of Flat Feet in Singapore
If you feel you have flat feet, see a podiatrist for an accurate diagnosis. The podiatrist will examine your feet and determine the extent of the deformity. This examination may include the use of 3D foot scans or X-rays. We have seen many patients who were told that they are flat-footed but are actually not. This is the reason why you should consult a Podiatrist always.
Treatment Options for Flat Feet in Singapore
Treatment for flat feet in Singapore depends on the severity of the condition. Additionally, the choice of treatment may also change if you are experiencing pain. Mild cases may be addressed with non-surgical options such as:
- Orthotics: custom-made shoe inserts can provide support for the arch and relieve pain
- Shockwave therapy: Shockwave therapies such as radial pressure wave therapy can help to relieve muscle tightness and fatigue caused by flat feet.
- Physical therapy: exercises can help strengthen the muscles in the feet and ankles
- Footwear: wearing shoes with good arch support can help alleviate pain and discomfort
In severe cases, surgery may be necessary to correct the flat foot deformity. However, this is only needed if non-surgical management options fails to help.
Prevention of Flat Feet in Singapore
Whilst most flat feet deformity cannot be prevented, preventing painful flat feet in Singapore is possible. You can try the following tips:
- Maintain a healthy weight to reduce the load on the feet
- Wear shoes that are correctly fitting and have sufficient support. (Read how to choose the right shoe for you)
- Perform foot and ankle exercises to strengthen the muscles in the feet
FAQs about Flat Feet
What are the causes of flat feet?
Flat feet can be caused by a variety of factors, including genetics, injury, and wear and tear over time. Some people are born with flat feet, while others develop them over time due to a variety of reasons, such as obesity, pregnancy, or ankle injury.
Can flat feet cause pain?
Flat feet can cause pain, especially if the condition is left untreated. The lack of arch support can cause strain on the muscles, tendons, and ligaments in the foot and leg, leading to pain and discomfort. Additionally, flat feet can cause other foot problems, such as plantar fasciitis and Achilles tendonitis.
How are flat feet diagnosed?
Flat feet can be diagnosed through a physical examination by a podiatrist or other healthcare professional. The healthcare professional will examine the foot and observe how it functions during movement. In some cases, imaging tests such as X-rays may be needed to further evaluate the condition.
How are flat feet managed?
Management options for flat feet typically involves non-surgical measures, such as custom orthotics, supportive footwear, and physical therapy. However, in severely painful cases, surgery may be necessary to correct the condition.
Can flat feet be prevented?
While most cases of flat feet cannot be prevented, pain can be prevented by maintaining a healthy weight, wearing supportive footwear, and engaging in exercises to strengthen the foot and ankle muscles.
Kesimpulan
Flat feet can cause pain and discomfort, but with proper diagnosis and management, it is a condition that can be alleviated. If you are experiencing pain or discomfort in your feet, it is important to see a healthcare professional for evaluation and treatment.
At Straits Podiatry, we specialize in diagnosing and managing a variety of foot and ankle conditions, including flat feet. Our team of highly skilled and experienced podiatrists is dedicated to providing personalized care to each of our patients. Contact us today to schedule an appointment and take the first step towards better foot health.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Understanding Ankle Sprains
An ankle sprain is a common injury that occurs when the ligaments in the ankle are stretched or torn due to excessive force or pressure. This can happen during physical activities like running, jumping, or sudden changes in direction. Ankle sprains can range from mild to severe, depending on the extent of the injury. Oftentimes, we have seen people seek ankle sprain treatment in Singapore without knowing that they had a fracture.
One of the biggest issues that many people face when they have an ankle sprain is who can help them. Treating an ankle sprain without proper diagnosis can be dangerous and may lead to worse consequences. In this article, we will share with what the symptoms of ankle sprains to look out for, the usual method of diagnosis and treatment, and ways to prevent it.
Symptoms of Ankle Sprains
The symptoms of an ankle sprain may vary depending on the severity of the injury. Among the most common symptoms are:
- Pain or tenderness in the ankle
- Bruising or swelling around the ankle
- Difficulty or inability to walk or bear weight on the affected foot
- Stiffness in the ankle joint

Diagnosis dan Rawatan
If you suspect that you have an ankle sprain or twisted your ankle, it is important to seek medical attention as soon as possible. A healthcare provider will examine your ankle and may order X-rays or other imaging tests to determine the extent of the injury. In serious cases, a complete ligament tear or fractures do happen, especially in sprains with severe bruising.
Treatment options for ankle sprains may include:
- Resting the affected ankle
- Applying ice and compression to reduce swelling
- Compression with a bandage or brace
- Elevating the affected foot
- Using over-the-counter pain relievers
- Doing exercises to improve flexibility and strength
- Using orthotics or other devices to support the ankle
- Shockwave therapy or magnetic field therapy to reduce pain and swelling
In severe cases, surgery may be necessary to repair the damaged ligaments. However, to regain proper ankle functions after surgery, rehabilitation is essential. This includes physical therapy, strength and conditioning, and gait training.

Preventing Ankle Sprains
While it may not always be possible to prevent ankle sprains, there are some steps you can take to reduce your risk of injury. These include:
- Wearing supportive shoes that fit well
- Using orthotics or other devices to support the ankle
- Doing exercises to improve strength and flexibility in the ankle joint
- Gradually increased the intensity of physical activities that place excessive stress on the ankle
- Complete a proper rehabilitation and re-training program after an ankle sprain so that a recurrence risk is minimised
Kesimpulan
If you’ve recently experienced an ankle sprain, seeking proper medical attention from a qualified healthcare provider is important. At Straits Podiatry, we specialize in the diagnosis and management of various foot and ankle conditions, including ankle sprains.
Our team of experienced podiatrists will work closely with you to develop a personalized management plan that meets your unique needs and goals. Depending on the severity, we offer the most appropriate ankle sprain management in Singapore. Management options may include rest, ice, compression, shockwave therapy and magnetotransduction therapy.
At Straits Podiatry, we are committed to helping you achieve optimal foot and ankle health, so you can get back to your daily activities as soon as possible. Contact us today to schedule an appointment and take the first step towards a full recovery.
Don’t let an ankle sprain hold you back – trust the experts at Straits Podiatry to provide you with the care and support you need to get back on your feet. Visit our website at straitspodiatry.com to learn more about our services and schedule your appointment today.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Foot corn removal is a standard medical procedure that many people in Singapore are seeking. Corns are small, thickened areas of skin that can develop on the feet and toes. They are often caused by friction or pressure and can be very painful and uncomfortable. Corns can be treated through a variety of methods, including home remedies, pressure offloading devices, and medical procedures. In this article, we will discuss foot corn removal in Singapore, including the different types of corns, causes of corns, and treatment options.
Types of Foot Corns:
There are three kinds of foot corn: hard corns, soft corns, and seed corns. Hard corns are the most common type and are usually found on the tip of the toes or on the soles of the feet. They are small, round, and have a hard centre core. Soft corns, on the other hand, are found between the toes and are usually moist and soft. Seed corns are tiny little cores of hard skin that can cause pin-pricking pain.

Causes of Foot Corns:
High friction or pressure on the feet is the main cause of corns. This can be due to wearing tight shoes, high heels, or shoes that are too small. Other factors that can contribute to the development of corns include foot deformities, such as hammertoes or bunions, flat feet, and activities that put repetitive pressure on the feet, such as running or walking long distances.
Foot Corn Treatment Options:
There are several options available for foot corn removal in Singapore. The most common methods include:
- Home remedies – These are the most cost-effective and easiest methods to try before seeking medical attention. Home remedies include applying moisturiser regularly, using a pumice stone to file down the corn, and wearing good-fitting footwear.
- Medical procedures -If the corn is painful or severe, seek medical treatment. Podiatrists often perform foot corn removal in Singapore using a scalpel.
- Pressure offloading devices – Medical devices such as customised insoles can help to reduce pressure and friction on the feet and toes. This can reduce the growth rate of the corns.
- Surgical removal – Only needed if the corn is very severe and nothing else worked. However, surgical removal does not guarantee that the corn will not return.

Foot Corn Removal Options in Singapore that You Should Avoid:
- Over-the-counter products – There are various products available at drug stores that claim to remove corns, such as foot corn removal plasters or salicylic acid ointment. However, misusing such products can cause deep burns and wounds.
- Do-it-yourself foot corn removal – Trying to remove foot corns on your own (e.g using scissors or penknife) can cause deep cuts and risk developing bacterial infections.
Foot Corn Prevention:
To prevent corns from developing, it is important to choose shoes that fit properly and are comfortable. Avoid wearing high heels for long periods and choose shoes with wider toe boxes. It is also important to avoid doing high-impact exercises barefoot.
In conclusion, if you are experiencing painful corns on your feet, it is essential to take prompt action to alleviate the pain and discomfort they cause. From simple home remedies to more complex medical procedures, there are various options for foot corn removal in Singapore.
To get the best advice and management for your condition, we recommend you consult a qualified podiatrist. At Straits Podiatry, we offer personalized and effective solutions for all types of foot problems, including corns. Contact us today to schedule an appointment. Visit straitspodiatry.com for more information.
Dikarang dan disunting oleh Straits Podiatry
FAQs on Foot Corn Removal
Foot corn removal is usually painless except for severe cases. Severe cases where the core of the corn is very deep, slight discomfort may be felt during the foot corn removal process. Your podiatrist will normally speak to you during the process to make the corn management as comfortable as possible.
Yes, it is. However, it is only possible to stop corn from growing when the underlying cause is properly addressed. High pressure and friction under the foot are the main causes of corn formation. Carefully designed customised insoles can often help to reduce the pressure and friction, thereby stopping the corn from growing.
Corns are thick layers of hard skin with a deep core in their centre. The core is visible when the layers of hard skin are removed. The core is responsible for causing sharp-pricking pain when you walk or stand on the corn. Calluses, on the other hand, are just layers of hard skin without a central core. Calluses are normally less painful unless it becomes very thick.
They are unfortunately not effective. Corn plasters contain salicylic acid and can cause burns on the skin. They do not reduce pressure or friction under the foot, hence they are unable to treat the corn effectively. Misusing these corn plasters can cause deep infections, so it is best to avoid them.
Freezing is not designed to remove or treat corn. Freezing is a treatment used for treating warts instead. If your corns have been treated with freezing, it is best to seek an expert to help you.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
When it comes to our overall health, many people overlook the importance of taking good care of our feet. We use our feet every day to stand, walk, and perform other physical activities, which can take a toll on them over time. Foot problems can lead to discomfort, pain, and even disability if left untreated. This is where podiatry comes in.
Podiatry is a branch of medicine that focuses on the diagnosis, management, and prevention of conditions affecting the feet, ankles, and lower extremities. A podiatrist, also known as a foot doctor, is a medical professional who specializes in this field. In Singapore, there are many foot specialists who can provide expert care for your feet. In this article, we’ll take a closer look at podiatry and the role of foot specialists in Singapore.
Some of the most common foot problems that podiatrists can help with include:
- Athlete’s foot: a fungal infection that affects the skin on the feet and toes
- Bunions are bony bumps that develop on the big toe’s joint.
- Plantar fasciitis: inflammation of the thick band of tissue that runs across the bottom of the foot
- Heel spurs are bony growths that occur on the heel bone.
- Ingrown toenails: a condition where the toenail grows into the skin, causing pain and inflammation
- Neuromas: a thickening of the tissue around a nerve in the foot, causing pain and discomfort
These are just a few examples of the many foot problems that podiatrists can diagnose and manage. They can also provide advice on how to prevent foot problems from occurring in the first place. For example, wearing properly-fitted shoes and practising good foot hygiene.
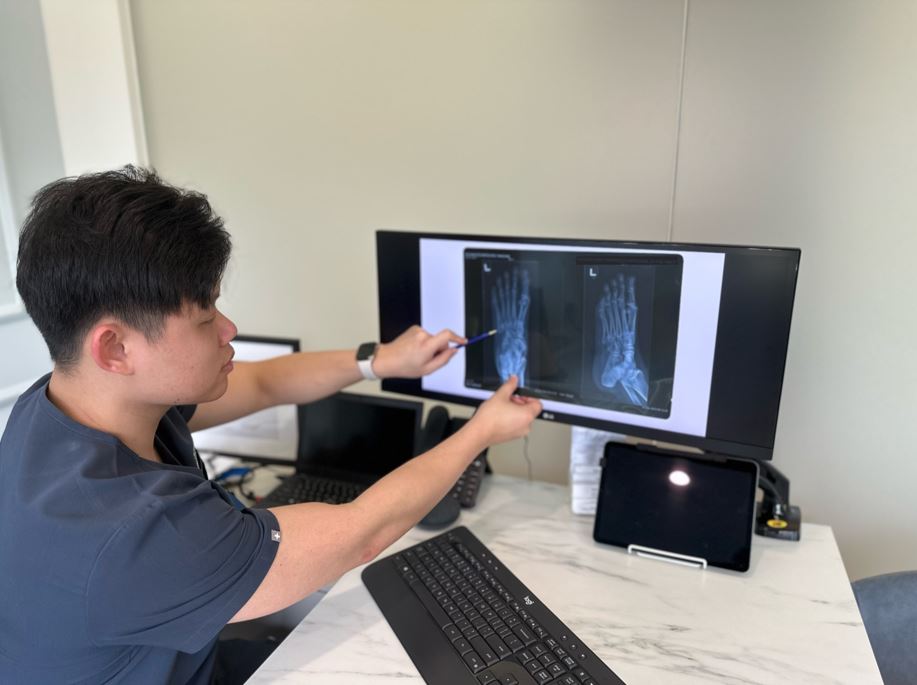
The Role of Foot Specialists in Singapore
In Singapore, there are many foot specialists who can provide expert care for your feet. These professionals are trained to diagnose and manage a wide range of foot problems. These can range from minor issues to more serious conditions.
One of the key benefits of seeing a foot specialist in Singapore is that they can provide personalized care tailored to your specific needs. They will take the time to understand your symptoms and medical history, and then develop a management plan that is right for you.
Foot specialists in Singapore use the latest technology and techniques to provide effective management for foot problems. They may use diagnostic tools such as X-rays, MRI scans, and ultrasounds to get a better understanding of the problem. Treatment options may include medication, advanced therapy, orthotics, and other devices.
In addition to providing management for foot problems, foot specialists in Singapore also place a strong emphasis on preventative care. They can provide advice on how to take good care of your feet, such as by wearing proper shoes, maintaining good foot hygiene, and exercising regularly.
Overall, foot specialists in Singapore play an important role in maintaining the health and well-being of the population. They provide expert care for a wide range of foot problems, helping people to live a more comfortable and active life.
Seek Help from Podiatrists
In conclusion, podiatry is a crucial medical specialty that focuses on the diagnosis, management, and prevention of conditions that affect the feet, ankles, and lower extremities. For individuals residing in Singapore, it is essential to have access to expert foot specialists who can provide comprehensive care for various foot problems ranging from minor issues to more severe conditions.
At Straits Podiatry, we are committed to delivering top-notch podiatry services to our clients in Singapore. To learn more about our services and how we can help you achieve optimal foot health, visit our website at straitspodiatry.com. Take the first step towards healthy feet and book your appointment with our local podiatry experts today.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Pengenalan
The Achilles tendon is one of the most crucial components of the foot’s anatomy. Often described as the powerhouse of the foot, the Achilles tendon plays a vital role in various forms of movement. Let’s look further into the essential functions of this tendon and its significance in maintaining foot health.
What is the Achilles Tendon?
The Achilles tendon is a strong, fibrous cord that connects the calf muscles (gastrocnemius and soleus), to the heel bone (calcaneus). It is the largest and also the strongest tendon in the human body, capable of withstanding forces of up to 1,000 pounds.
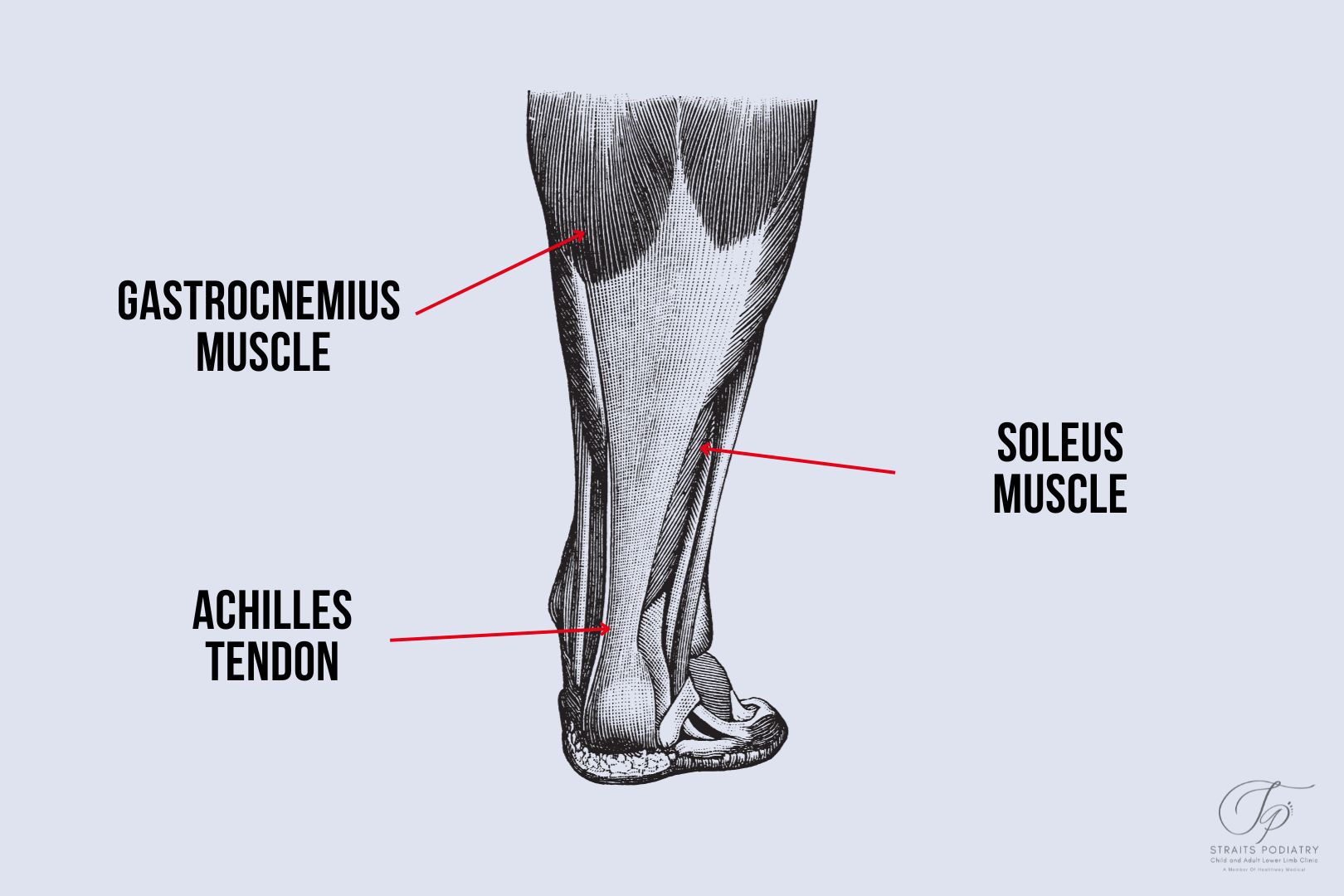
Functions of the Achilles Tendon
Powering Movement
The Achilles tendon is instrumental in powering the foot’s movement. It allows you to point your toe downwards, an action known as plantarflexion. This is essential, particularly in activities that involve the heel lifting off the ground, such as walking, running, and jumping. It is therefore the strongest driver during push-off.
Absorbing Shock
During activities like running or jumping, the Achilles tendon helps absorb the shock. It does so by contracting and lengthening at the same time, also known as an eccentric contraction. This slows down the speed of the force acting on our body, thereby reducing the impact on the heel and foot.
Enabling Balance
The Achilles tendon aids in maintaining balance by adjusting the foot’s position during movement, helping you navigate uneven surfaces. It also helps to balance the body’s centre of pressure by maintaining the body’s forward and backward sway.
Injury and Heel Pain
Similar to other body structures, the tendon can suffer too much stress and load, leading to inflammation and injury. This often results in conditions like Achilles tendinitis or Achilles rupture, both of which can cause significant heel pain.
Kesimpulan
The Achilles tendon is a vital component of the foot’s anatomy, playing a crucial role in powering movement, providing flexibility, absorbing shock, and enabling balance. Understanding its functions can offer valuable insights into foot health and preventing heel-related conditions.
Artikel Berkaitan
- Anatomi tumit: memahami struktur kompleks
- Perubahan Gaya Hidup untuk Mencegah Sakit Tumit di Persekitaran Bandar Singapura
- Mengapa saya mengalami sakit tumit?
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
As people age, their feet tend to experience more wear and tear, which can lead to various foot problems. A podiatrist is a healthcare professional who specialises in the diagnosis, management, and prevention of foot, ankle, and lower leg problems. They are also known as foot doctors, and they play an essential role in maintaining the overall health and well-being of the feet and the rest of the lower limbs. In Singapore, not many people know what services a podiatrist provide.
Therefore in this article, we will discuss the services provided by podiatrists and how they can help you maintain healthy feet.
Diagnosis and Management of Foot Injuries
Podiatrists are trained to diagnose and manage a wide range of foot and ankle injuries, including sprains, fractures, and dislocations. They are trained in various diagnostic tools such as ultrasound, X-rays, and MRI scans to identify the problem and develop a management plan that best suits your needs.
In addition to providing immediate care, podiatrists also work with patients on long-term solutions to prevent further injuries and improve overall foot health.

Management of Foot Deformities
Foot deformities such as bunions, hammertoes, and flat feet can cause significant discomfort and affect your mobility. A podiatrist can offer a range of management options, including custom orthotics, braces, and manual therapies to relieve pain and improve functions.
In some cases, surgery may be offered by orthopaedic surgeons. A podiatrist can also provide post-surgical support to improve the function and appearance of your feet.
Management of Skin and Nail Conditions
Podiatrists also diagnose and manage a variety of skin and nail conditions affecting the feet. These may include fungal infections, warts, and ingrown toenails. They use different methods to manage these conditions, including medication, laser therapy, and surgery.
In addition to management solutions, podiatrists also offer advice on proper foot hygiene and care to prevent future infections and conditions.
Diabetic Foot Care
People with diabetes are at a higher risk of developing foot problems due to poor circulation and nerve damage. Podiatrists play a crucial role in preventing and managing foot problems in people with diabetes.
They conduct regular foot exams to identify any issues early on and develop a comprehensive care plan. That normally includes regular checkups, proper foot hygiene, and education on how to prevent foot problems.
Sports Injury Management and Prevention
Podiatrists also work with athletes to diagnose and manage sports-related foot and ankle injuries. The type of injuries ranges from calf or hamstring strains to tendon injuries or fractures. They can also provide advice on injury prevention and tips on selecting proper footwear. This is to improve athletic performance and reduce the risk of injury.
Kesimpulan
In conclusion, a podiatrist is a specialised healthcare professional who can diagnose, manage, and prevent a wide range of foot and ankle problems. From injuries to deformities, skin and nail conditions to diabetic foot care, and sports-related injuries, podiatrists offer comprehensive care for healthy feet.
If you are experiencing any foot problems, it is essential to seek the advice of a podiatrist. At Straits Podiatry, we help you identify the problem and develop a personalised management plan. Our goal is to get you back on your feet and maintain optimal foot health.
If you want to know more about the services our Podiatrists can provide, contact us today!
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
At some point in life, everyone has experienced a callus. Calluses are rough and hardened patches of skin that form due to repeated friction or pressure on a specific area of the skin. They can appear on any part of the body but are commonly found on the hands, feet, and elbows. Although they are rarely harmful, they can be unsightly and uncomfortable. They can also cause great pain when it is left untreated. Therefore, it is essential to get proper callus treatment from a professional to avoid any discomfort.
If you are looking for callus management in Singapore, you have come to the right place. We are a team of experienced professionals who provide a comprehensive range of foot callus solutions that will leave your skin smooth and healthy.

Understanding Calluses
Before we dive into the management options, let us first understand what calluses are and how they form. Calluses occur when the skin cells on a specific area of the body start to multiply rapidly, forming a thick, hardened layer of skin. Generally, the primary cause of calluses is repeated friction or pressure on the skin. Some common causes of calluses include wearing tight-fitting shoes, walking or standing for extended periods, foot deformities such as clawed or hammertoes, and weightlifting.
Callus Treatment Options
- Soak and Scrub: Soaking and scrubbing the affected area is one of the easiest and most effective ways to treat calluses. Soaking the skin in warm, soapy water for about ten minutes will help soften the callus, making it easier to remove. After soaking, gently scrub the area with a pumice stone or a foot file to remove the dead skin. It is essential to be gentle and not scrub too hard, as this can cause bleeding and risk having infections.
- Moisturize: Keeping the skin moisturized is essential in preventing and treating calluses. Applying a moisturizer to the affected area can help soften the skin, making it easier to remove the dead skin. It is best to use a moisturizer that contains urea it can help break down the thick, hardened layer of skin.
- Medications: If the callus is particularly stubborn, your doctor may prescribe a medication to help soften the skin. Salicylic acid is a common medication prescribed to treat calluses. It basically works by dissolving the protein that holds the dead skin together, making it easier to remove. However, this is not usually recommended because it can cause deep burns if used incorrectly.
- Medical management: If your callus is bothering you, seek help from a Podiatrist. Podiatrists can help to remove the callus using a scalpel. Generally, they will also advise on shoes and customised insoles to help reduce the pressure on the callus area.
Why Choose Us for Callus Management in Singapore?
At our clinic, we understand that every patient is unique, and we tailor our management to meet their individual needs. Our team of experienced professionals uses the latest technology and techniques to provide safe and effective callus relief. We believe in providing our patients with a comfortable and welcoming environment, where they can feel at ease and confident in their management options.
If you are looking for effective callus solutions in Singapore, look no further than Straits Podiatry. Our experienced team of podiatrists provides a range of safe and effective management solutions that are tailored to meet your individual needs. From standard callus removal to advanced pressure-offloading solutions, we use the latest technology and techniques to provide you with the best possible care.
At Straits Podiatry, we are committed to ensuring your complete satisfaction. Our clinic is equipped with state-of-the-art facilities, and we maintain the highest standards of hygiene and safety. Our friendly and knowledgeable staff is always on hand to answer any questions you may have about your management plan.
Don’t let calluses make you uncomfortable or self-conscious. Contact us today at straitspodiatry.com to schedule an appointment and experience the difference in quality care. Let us help you get the healthy, smooth skin you deserve.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
As a healthcare profession, podiatry is an area of specialty that focuses on the study, diagnosis, and management of disorders and injuries of the feet and lower limbs. It is a crucial field of medicine that helps individuals maintain their mobility, avoid long-term disability, and improve their overall quality of life. But is podiatry recognised in Singapore? Let’s delve into the subject to find out.
Understanding Podiatry
Podiatry is a specialized medical field that deals with the assessment, diagnosis, and management of issues affecting the feet and lower limbs. It involves the use of specialized techniques and equipment to help patients manage foot-related conditions, such as fungal infections, foot deformities, heel pain, and diabetic foot care.
In many countries, podiatry is a recognized profession that requires specialized training and certification. However, its recognition varies from country to country, and this can impact its accessibility to patients who need it.

Podiatry in Singapore
In Singapore, podiatrist is recognized as an allied health professional by the Ministry of Health. The Podiatry Association (Singapore) was also formed in 1994 to set a common code of conduct and standards of practice for podiatrists in Singapore.
To practice as a podiatrist in Singapore, one must hold a degree in podiatry from a recognized overseas institution. This ensures that only qualified professionals can provide podiatry services in Singapore, giving patients peace of mind and making sure that they receive quality care.
Podiatry Services in Singapore
In Singapore, podiatry services are available in various settings, including private clinics, hospitals, and community health centres. Podiatrists also work closely with other healthcare professionals to provide comprehensive care to patients. They include orthopaedic surgeons, vascular surgeons, endocrinologists, rheumatologists, physiotherapists, and diabetes educators.
Some of the services provided by podiatrists in Singapore include:
- Foot and ankle assessments
- Management of foot and ankle injuries
- Custom-made orthoses
- Penjagaan kaki diabetes
- Management of nail and skin conditions
- Gait analysis and correction
Benefits of Podiatry in Singapore
Podiatry services play a vital role in the overall healthcare system in Singapore. By recognizing podiatry as a profession and providing access to qualified practitioners, Singaporeans can enjoy the following benefits:
- Improved foot health: Podiatrists help individuals maintain good foot health, prevent foot problems, and manage existing conditions.
- Better mobility: Individuals with foot and ankle problems can benefit from podiatry services, which can help improve their mobility and quality of life.
- Preventative care: Podiatrists can identify and manage foot problems before they become severe, preventing long-term complications and disability.
- Comprehensive care: Podiatrists work closely with other healthcare professionals to provide comprehensive care to patients with complex medical conditions.
Kesimpulan
In conclusion, podiatry is recognized as a healthcare profession in Singapore. Individuals can access quality podiatry services in Singapore from qualified professionals. The Podiatry Association (Singapore) also has a code of conduct and standard of practice for podiatrists. Basically, this is to make sure that patients can receive safe and quality podiatric care.
If you’re looking for professional and qualified podiatrists in Singapore, look no further than Straits Podiatry. Our team of experienced podiatrists are dedicated to providing quality care to help you maintain good foot health and improve your mobility.
Contact us through our website at www.straitspodiatry.com to learn more about our services and schedule an appointment. Don’t let foot problems hold you back from enjoying life to the fullest. Let us help you take the first step towards better foot health.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Pengenalan
Your feet are an essential part of your body. They support your weight, help you walk and run, and allow you to play sports. The bones in your feet are connected by ligaments and tendons, which can be injured if you have poor foot posture or wear improper footwear. Knowing when you should see a podiatrist (foot doctor) can help you prevent foot and ankle injuries in long run. Some podiatrists in Singapore are also trained to manage conditions of the leg, knee, and hip.
Getting treatment for your foot or ankle problem is important as soon as you suspect something is wrong. This way, you can keep your feet healthy and avoid further complications.
Here are some situations when you should see a podiatrist or a foot doctor:
A foot injury or pain that won’t go away.
If you have foot pain, it’s important to see a podiatrist. The foot can be affected by many different things, including injuries and conditions like arthritis.
Injuries include conditions such as strains, sprains, and fractures. An overuse injury also occurs from wearing worn-out shoes or high heels that are too high for an individual’s biomechanics.
A podiatrist can help you identify the cause of your pain and develop a management plan tailored to your needs.
Trouble walking, running, or even standing for long periods.
If you’re having difficulty walking or running because of soreness in your feet, then you should see a podiatrist. This could be due to an injury such as plantar fasciitis, an inflammation of the tissue on the bottom of your foot that connects your heel bone to your toes.
Plantar fasciitis is often caused by overpronation (rolling inward) when walking or running on hard surfaces such as concrete or asphalt for long periods without proper footwear. Proper footwear can help reduce the pain caused by overpronation and prevent further damage from occurring to your feet and ankles.
If you have an injury that doesn’t heal or pain that won’t go away, make an appointment with your podiatrist.

Your foot has been sprained or fractured in the past.
The most common foot injuries are sprains, strains, and fractures. A sprain is an injury to your foot’s ligaments (tissues that connect bones). A strain is when you injure your muscles or tendons which are tissues that connect muscle to bone. And a fracture involves broken bones in your foot.
If you have injured your foot in the past, it is important to see a podiatrist to ensure that it heals properly and that there are no complications.
You have bunions, hammertoes, corns, calluses, or other painful conditions on your feet.
Bunions, hammertoes, and corns are common foot problems that your podiatrist can manage.
Bunions are bony protrusions that form at the base of your big toe and can cause pain, swelling, and stiffness. They often occur in people with foot deformities such as hammertoes.
Hammertoes occur when toes bend into an abnormal position and curve toward each other or toward your other toes. They’re typically caused by tight shoes that exert too much pressure on them over time.
Corns (also known as calluses) form when the skin grows thicker than normal due to friction between two surfaces rubbing together–like heels rubbing against shoe insoles or between toes inside socks or boots that don’t provide enough room for them all to move freely without touching each other.
If shoes feel too tight or pinch in certain spots on your feet.
Shoes that are too large can cause blisters and calluses. If you have to wiggle your toes around inside the shoe to get it to fit comfortably (and even then, it doesn’t feel right), try a different size shoe.
If you have a problem with shoes that don’t fit properly, see a podiatrist for an evaluation. A podiatrist will examine the condition of your feet and make suggestions about how to improve the fit of your shoes. If there is something wrong with the shoes themselves, he or she can recommend other options for you.
When you have an ankle sprain
An ankle sprain is a specific kind of injury that can happen to anyone. It happens when you over-stretch or tear one or more ligaments in your ankle joint. Ligaments, which bind bones together, are strong bands of tissue that keeps the bones stable. When they get hurt in the ankle, it’s called an ankle sprain.
Ankle sprains are common and usually happen during sports activities like basketball, football, and running. They can also be caused by tripping on uneven ground or staircases while walking around at home or school.
To prevent an ankle sprain: Wear good shoes with good support; wear shoes designed for the sport you are doing; warm up before exercising; stay away from exercising on wet uneven grounds.
You have a reoccurring case of an athlete’s foot.
If you have a reoccurring case of an athlete’s foot, it could be a sign that there is something wrong with your feet or health. If left untreated, an athlete’s foot can cause serious infections in the bloodstream, joints, and bones. A podiatrist can also tell you if the skin problem is indeed an athlete’s foot or other conditions.

You have nail fungus.
If you have nail fungus, it means that there is an infection in the area under your nail. The fungus causes discolouration and thickening of the nails, and possibly pain if left untreated.
Nail fungi can be caused by trauma to the nail or from wearing shoes that are too small or tight. They can also spread from person to person through sharing shoes or towels. You could also catch the infection from going to pedicures regularly. While they cause an infection in the toenails (particularly big toes), they can also spread and affect any part of your foot, including:
- The skin around your nails
- The skin between the toes
If you have feet or toenails fungal infections, it’s important that you see your podiatrist for a management plan. Your podiatrist may use special tools, such as light therapy (known as PACT), in addition to medications and other solutions for nail fungus removal.
When you have an ingrown toenail
One of the most seen issues with the feet is ingrown toenails which can be very painful, so it’s best to see a podiatrist as soon as possible. You can cause yourself a serious infection if it is left untreated. Your podiatrist may file down the nail or cut away part of it in order to relieve some of your pain. In worse cases, your podiatrist could also manage the ingrown toenail for good by doing a procedure.
Joint pain in the foot or ankle
Joint pain in the foot or ankle can be caused by many things, including arthritis, injury, and overuse. If you have joint pain in your foot or ankle, it’s important to see a podiatrist for an evaluation.
If you notice any symptoms of knee joint problems, such as tenderness when walking, swelling and warmth around the affected area, and stiffness when getting out of bed, then these may indicate early knee osteoarthritis. Osteoarthritis occurs when cartilage breaks down due to wear and tear on joints that causes them to lose their smoothness — like an old shoe losing its lustre after years of use.
Kesimpulan
Podiatrists are foot doctors and lower limb health experts. Whilst they are known as foot doctors, they can also take care of various problems that you may have related to the foot, ankle, leg, knee, and hip. Podiatrists can provide solutions for issues related to pain in the bones, joints, muscles and tendons. They can also provide care for your skin and nails. So if you are experiencing any foot, ankle, leg or knee problems, the best thing to do is to call your podiatrist. They will be able to give you the proper diagnosis and management plan for your condition.
If you have any questions about when you should see a podiatrist or a foot doctor, please feel free to contact us here. At Straits Podiatry, we have a highly experienced team of podiatrists in Singapore that can tailor the management plan to your needs. If you need more information about Podiatrists or foot doctors in Singapore, you may wish to visit our association.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Are you experiencing discomfort in your foot or ankle? It’s crucial to address these issues by seeking professional medical attention. One specialist who can assist you is a podiatrist. Nevertheless, discovering the ideal podiatrist can be a daunting task. Here’s a comprehensive guide to assist you in finding the best podiatrist in Singapore.
Apa itu Podiatry?
Podiatry is a branch of medicine or allied health profession that focuses on the prevention, diagnosis, and management of conditions affecting the feet, ankles, and lower legs. Podiatrists, also known as foot doctors, are trained to deal with a wide range of foot and ankle problems, including:
- Kecederaan sukan
- Sakit tumit
- Kuku jari kaki yang tumbuh
- Jagung dan calluses
- Kaki rata
- Bunions
- Artritis
- Masalah kaki diabetes
- Fasciitis plantar
- Fractures and dislocations
Podiatrists are also trained to provide preventive care, such as teaching patients about maintaining good foot health. They can also prescribe orthotics or recommend exercises to improve foot and ankle strength.

Why Should You See a Podiatrist?
If you’re experiencing foot or ankle pain or problems, it’s important to seek the help of a qualified health professional. A podiatrist is an expert who deals with the diagnosis, management, and prevention of conditions affecting the feet, ankles, and lower legs. Here are some reasons why you should consider seeing a podiatrist:
1. Foot and Ankle Pain
If you’re experiencing foot or ankle pain, a podiatrist can help diagnose the problem and recommend the appropriate solution. Whether you have heel pain, plantar fasciitis, or an ankle sprain, a podiatrist can provide the care you need to get rid of pain and restore function.
2. Diabetic Foot Care
If you have diabetes, you’re at high risk of developing foot problems such as neuropathy, infections, and ulcers. A podiatrist can provide education and solutions to help manage these conditions and reduce the risk of complications.
3. Sports Injuries
Whether you’re an amateur or a professional athlete, sports injuries are common. A podiatrist can provide specialized care for sports-related foot and ankle injuries, such as ankle sprains, stress fractures, and Achilles tendonitis. Besides management, a podiatrist can also provide education and guidance on how to prevent injuries when doing sports such as running.
4. Ingrown Toenails
Ingrown toenails can be painful and can lead to infection if it is not treated. A podiatrist can provide management solutions to relieve pain and prevent infection, and can also recommend steps or ways to reduce the risk of future ingrown toenails. In addition, they can perform a partial nail avulsion to relieve the ingrown toenails permanently.
5. Custom Orthotics
If you have foot or ankle problems, such as flat feet or high arches, custom orthotics can help provide support and reduce pain. Generally, a podiatrist can provide a thorough evaluation and recommend appropriate orthotics to meet your needs.
6. Nail and Skin Problems
Podiatrists can also provide care for nail and skin problems of the feet and ankles, such as fungal infections, plantar warts, and calluses. They can also provide solutions to get rid of the pain and prevent the problem from getting worse.
Factors to Consider When Choosing the Best Podiatrist Near You in Singapore
When searching for the best podiatrist in Singapore, there are several critical factors to keep in mind, here are some of the most important factors to consider:
Qualifications and Credentials
It’s important to choose a podiatrist who is licensed and certified by the relevant authorities in Singapore. Look for a podiatrist who has the appropriate qualifications and credentials, such as a Bachelor of Science in Podiatry or a Doctor of Podiatric Medicine degree.
Experience and Expertise
Experience and expertise are crucial when it comes to choosing a podiatrist. Therefore, look for a podiatrist with years of experience in managing foot and ankle problems and expertise in a specific area of podiatry. For example, if you’re dealing with sports-related foot injuries, look for a podiatrist specialising in sports podiatry.
Range of Services Offered
Choose a podiatrist who offers a range of services to meet your foot care needs. Look for a podiatrist who can manage a variety of foot and ankle conditions, including bunions, plantar fasciitis, and diabetic foot problems. Also, look for a podiatry clinic that has a great range of management options so that you are getting the best care for your problems.
Communication and Patient Care
It’s important to choose a podiatrist who is easy to communicate with and who takes the time to listen to your concerns. You should also look for one who prioritizes patient care and is dedicated to helping you achieve the best possible outcomes.
Reputation and Reviews
Before deciding, you should research the reputation of the podiatrist you’re considering and read reviews from other patients. Look for one who has a positive reputation and who has received positive reviews for their quality of care.
Location and Availability
Choose a podiatrist who is conveniently located and has office hours that work with your schedule. This can certainly make it easier to get the care you need without disrupting your daily routine.
Kesimpulan:
Finding the best podiatrist near you in Singapore may seem like a daunting task, but it’s worth the effort to ensure you receive the best possible care for your foot or ankle problem.
At Straits Podiatry, we are dedicated to providing the highest level of care to our patients. Our team of experienced podiatrists uses the latest technology and techniques to diagnose and manage a wide range of foot and ankle problems. Whether you’re dealing with plantar fasciitis, bunions, heel spurs, ingrown toenails, or sports injuries, we can help.
Don’t let a foot or ankle pain hold you back. Take the first step towards recovery by getting a consultation with Straits Podiatry today. Visit our website at straitspodiatry.com to learn more about our services and to book an appointment.
Soalan lazim:
Choosing a good podiatrist involves several factors. Here are some things to consider:
i. Qualifications: Look for a podiatrist who is licensed and has the necessary qualifications and certifications.
ii. Experience: Find out how long the podiatrist has been practising and what their area of expertise is.
iii. Services offered: Consider the range of services the podiatrist offers, and whether they can meet your specific needs.
iv. Location: Choose a podiatry clinic that is conveniently located and easily accessible.
v. Reputation: Read reviews and ask for referrals from friends, family, or your primary care physician.
One of the most common problems managed by podiatrists is heel pain, specifically plantar fasciitis. Other common conditions managed by them include bunions, corns and calluses, and ingrown toenails.
A foot doctor and a podiatrist are essentially the same things. Basically, both terms refer to a medical specialist who manages conditions of the foot and ankle. However, the term podiatrist is more commonly used in the medical field.
Podiatrists possess the expertise to identify and address a diverse array of foot and ankle issues, spanning a broad range of conditions such as:
i. Plantar fasciitis
ii. Bunions
iii. Corns and calluses
iv. Ingrown toenails
v. Fungal nail infections
vi. Achilles tendonitis
vii. Heel spurs
viii. Flat feet
ix. Neuromas
x. Diabetic foot problems
In addition to these conditions, they can also provide preventative care and advise on proper foot care techniques to help avoid future problems.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Heel pain is, by far, the most common foot pain problem that we see in the clinic daily. Many of our patients would tell us that they tried several home remedies, but they did not help. The reason is that you need to know what is causing your heel pain to know the best way to resolve it. There are several reasons why your heel is painful. Here are some possible causes:
1. Plantar fasciitis
Plantar fasciitis is one of the most common causes of heel pain. It occurs when the band of tissue that runs from your heel to your toes becomes inflamed. Plantar fasciitis is often caused by flat feet, high arch feet, long standing hours, or poor footwear. The classic symptom of plantar fasciitis is a sharp stabbing pain that is worse in the morning or after periods of rest.
2. Achilles tendinitis
Achilles tendinitis is another common cause of heel pain, which occurs when the Achilles tendon becomes inflamed. The Achilles tendon runs from the back of the leg (calf muscle) down to the heel bone. Achilles tendinitis is often caused by excessive high-impact sports such as running or jumping. It can cause dull or sharp pain in the back of the heel and is often worse after exercise.
3. Heel spurs
Heel spurs are bony growths that form on the bottom or the back of the heel bone. They often occur as a result of long-term plantar fasciitis or Achilles tendinitis. Heel spurs are our body’s natural response to tendon stress, and they are usually not the main cause of your heel pain. The symptoms of heel spurs are largely similar to plantar fasciitis or Achilles tendinitis, depending on where the spurs are at.

4. Stress fractures
Stress fractures are tiny cracks in the bone that can occur as a result of overuse or repetitive stress. Individuals that often get heel stress fractures are long-distance runners or jumping sports. They can cause sharp pain in the heel that is worse during exercise. Stress fractures can also occur and cause foot pain in other parts of the foot.
5. Retrocalcaneal Bursitis
Retrocalcaneal bursitis is the inflammation of the bursa, a small fluid-filled sac that cushions and reduce the friction between the Achilles tendon and the heel bone. Retrocalcaneal bursitis typically affects athletes such as football or basketball. It can cause heel pain that is worse with movements such as running uphill or sprinting.
Getting the right diagnosis is the key to recovery
There are other less common causes of heel pain, such as nerve entrapment or systemic diseases like rheumatoid arthritis. So, as you can see, there are many conditions that cause heel pain in Singapore. The solution for heel pain only works if the diagnosis is correct. If you have been suffering from heel pain for some time, it’s best to consult with a podiatrist for appropriate assessment and management. Our podiatrists at Straits Podiatry are experienced in managing various conditions and we often see many cases of common foot and ankle pain. Hence, if you need help finding the best podiatrist in Singapore, call us today and let us assist you!
If you enjoy reading this article, please feel free to share the knowledge with your friends. We will regularly create more content related to lower limb health, so follow us on our Facebook page or Instagram to stay updated!
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Our feet and ankle are complex structures that are so carefully designed to withstand our body weight and even higher loads when we stand and move about daily. Therefore we should take good care of our feet, otherwise, they are prone to injuries. Here are five of the most common foot and ankle injuries that we see in our clinic:
1. Ankle Sprain
Ankle sprains are a common ankle injury that occurs when the ankle overly twists inwards or outwards. The ligaments in the ankle often become stretched or torn, resulting in redness, swelling, and stiffness of the ankle. Sports that involve many twisting and turns such as basketball or football are common causes of ankle sprains. We often see patients try to “walk it off” instead of seeking medical attention and that is not ideal. Ankle sprains must be treated carefully because up to 40% of cases suffer from chronic symptoms and repeated sprains. Therefore, we highly recommend a structured rehabilitation program to prevent future sprains or chronic ankle instability.

2. Achilles Tendonitis
Achilles tendonitis is usually an overuse foot and ankle injury caused by inflammation in the Achilles tendon, which connects our calf muscles to the heel bone. Runners and athletes of jumping sports are at risk because of the repetitive stress on the Achilles tendon. Achilles tendonitis causes pain, redness, and swelling at the back of the heel or ankle, and you will also find difficulty standing on the toes. We typically recommend a combination of solutions and strengthening exercises to manage Achilles tendonitis.
3. Plantar Fasciitis
Plantar fasciitis is the most common foot injury that causes heel pain. It occurs when the plantar fascia, a band of tissue that supports the arch of the foot, becomes inflamed. The typical causes of plantar fasciitis that we see include flat feet, incorrect choice of footwear, and poor training form. We normally manage plantar fasciitis by managing both the inflammation and the root cause of the condition.
4. Posterior Tibial Tendonitis
Posterior tibial tendonitis is a common foot and ankle injury caused by inflammation and weakening of the posterior tibial tendon. The posterior tibial tendon helps support our arch and stabilise our foot during propulsion. Posterior tibial tendonitis typically occurs in runners or jumping sports and especially in people with flat feet. We normally manage posterior tibial tendonitis with customized foot orthoses or ankle-foot orthoses depending on the severity.
5. Stress fractures
Stress fractures are small hairline cracks in the bone that are caused by overuse or repeated stress. They usually happen in the foot or ankle, especially the forefoot. Stress fractures usually occur in athletes who take part in high-impact sports. Other common causes include a poor choice of shoes when doing sports and inadequate recovery. Stress fractures often take between 4 to 6 weeks to recover but management such as shockwave therapy may help to speed up recovery.
Prevention is better than cure
It is important to understand that our feet and ankle normally get injured when the stress is too much to bear. We can prevent injuries with the right choice of footwear and proper training techniques (read how you can prevent injuries while running). If you are experiencing any pain in your foot or ankle, consult with our Podiatrists at Straits Podiatry and get relief early today.

Since the start of the COVID-19 pandemic, more people have picked up running as a sport to maintain good health. Whilst it is a highly recommended action to take, we also noticed an increased number of lower limb injuries because of running. So here are some tips to help you prevent any lower limb injuries when running:
1. Start with a proper warm-up
Warm-up exercises are important! A proper warm-up raises your heart rate and gets your blood circulation going. A common misconception that people have is to stretch before running, and that is incorrect. Before you start running, do some active movements such as forward or lateral leg swings, forward and backward lunges, and supported squats. A short jog on the spot for a minute before the start of the run would be good too!
2. Wear proper shoes
Proper running shoes will help you a long way in preventing running injuries. But the question is, how do I know which shoes are good for me? The general rule is to always make sure you wear running shoes that fit well and are designed for your foot type and running style. Technology advancements have led to the creation of running shoes designed to enhance performance; however, remember that it does not necessarily mean those shoes are suitable for everyone!
3. Increase your mileage gradually
A sudden increase in activity often leads to common lower limb overuse injuries. Therefore, you should avoid increasing your running mileage too quickly. Gradually increasing your mileage by 10 to 15% per week would be ideal. Take note that increasing your speed or frequency of training is also increasing your intensity of activity!

4. Cross-training with other exercises
An effective way to reduce muscle overuse and prevent running injuries is to incorporate other forms of exercise. Try cross-training with activities such as swimming, cycling, or strength training. The muscular demands for each activity are different, therefore it gives your muscles a break to recover!
5. Listen to your body
The most common reply that we hear from patients is “it used to be just a little bit of pain, but I thought it will go away”. And the pain did not go away, it became worse with continuous training. If you feel pain or discomfort while running, stop and take a break. A mild strain such as a hamstrings strain can take between 2 to 4 weeks to recover with rest. Ignoring pain can lead to more serious injuries.
6. Get sufficient rest
Our body has a limit to stress and beyond it, injuries occur. Making sure you give your body enough time to rest and recover between runs is an important step to prevent running injuries. This means taking at least one or two rest days per week, getting enough sleep, and considering recovery treatments such as massage or trigger point release.
7. Seek help from professionals
Mild lower limb injuries would often recover within a few weeks. If the pain or discomfort you are experiencing is not showing signs of getting better despite sufficient rest, consult with a sports podiatrist (meet our team of Podiatrists). If the problem is beyond the lower limbs, consult with a sports medicine doctor!
If you enjoy our content, do check back regularly to learn more about lower limb health and valuable tips! Check out our conditions page if you want to know more about a particular lower limb condition!
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Choosing the right type of shoe provides a range of benefits such as comfort, and support, and reduces the risk of foot injuries. However, most people find it difficult to select the right pair of shoes for their feet. So, here are some valuable tips from a Podiatrist:
1. Shoes for flat feet (Overpronators)
Individuals with flat feet have low or no arches, and their ankles roll inwards excessively (overpronation) when they walk. For mild-to-moderate flat feet, stability shoes are recommended as they are designed to reduce the amount of pronation. Reducing pronation helps to reduce the stress on our bones, joints, tendons, and muscles. For severely flat feet, look for shoes that have motion control features, such as a firm midsole, and a stiff heel counter to help stabilize your feet. Also, shoes for flat feet should come with a straight last (the shape of the shoe) to provide more support for your flat feet.
2. Shoes for high arch feet (Underpronators)
Individuals with high arch feet have well-defined arches such that only the heel and the ball of the feet touch the ground. For high-arch feet, we generally recommend shoes with good cushioning properties. Look for shoes with a curved last, which contours the foot and helps distribute pressure across the foot better. Adding cushioned insoles into the shoes can also help provide extra comfort.

3. Individuals with wider feet
Choosing the right shoe width can help prevent common foot conditions such as bunions and Morton’s neuroma. Individuals with wide feet should look for shoes with a wider toe box, such as shoes with a rounded or square toe box. Also, shoes with a softer upper can help accommodate the shape of your foot. It is essential not to buy a larger shoe size just to fit the width of your feet. Most people do not know that there are different sizes for the width. For ladies, wide-fitting shoes are labelled as “D” width, and for men, look for “2E” or “4E”.
4. Always try before buying
Everyone’s feet are unique, so it is essential to try on shoes and see how they feel before buying. Therefore, we generally do not recommend buying shoes online. If you have a specific foot condition, deformity, or injury, it is best to consult with a Podiatrist or healthcare professional for personalized shoe recommendations.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Our feet are the base and the foundation of our body and are responsible for enabling us to walk, run, jump, and even perform various movements comfortably. Each day, our feet support up to 120% of our body weight when walking, and upwards of 200% of our body weight when running. Because of this, injuries will occur if our feet are not cared for well enough. According to an American Podiatric Medical Association study, approximately 77% of people between the ages of 18 and 65 have suffered from foot pain at some time in life, and half of them find that the pain restricted their daily activities. To prevent this, you should go for a foot health screening regularly. Here are some benefits of going for foot health screening:
1. Early detection of foot problems
Regular foot health screenings can help detect foot problems early before they become severe. This can include issues like bunions, clawed toes, corns and calluses, and other minor issues that, if neglected, can lead to more significant problems.
2. Prevention of injuries
Foot health screenings can help you identify any issues with your feet that could put you at risk of developing foot injuries. Such issues are usually determined by assessing your foot posture and gait pattern. For example, if you have flat feet, you may be more prone to developing conditions such as plantar fasciitis or posterior tibial tendonitis. By identifying these issues early, you can take steps to prevent injuries from occurring.
3. Management of chronic conditions
If you have a chronic condition like diabetes or arthritis, regular foot health screenings are crucial. This is because foot health screening can help you manage and monitor any foot complications arising from these conditions. Diabetes, for example, can cause nerve damage and reduced circulation in the feet. As a result, it can cause numbness of the feet and poor wound healing. Regular foot health screenings can help you identify these issues early so that you can take steps to manage them.

4. Improved lower limb mobility
Foot problems impact your ability to move around comfortably. By identifying and addressing foot issues early, you can improve your mobility and enjoy doing your favourite sport. For elderlies, improving mobility means a reduced risk of falls.
5. Professional footwear advice
Foot health screenings can help you identify the best type of footwear for your feet. Through the assessment, your Podiatrist can provide a range of recommended footwear that would likely suit your feet. This can help reduce the risk of foot problems and improve your overall foot health.
Go For A Foot Health Screening Today
Overall, foot health screenings are essential to maintaining good overall health. This is because they can help you identify any foot problems early, prevent injuries, manage chronic conditions, improve mobility, and help choose the best footwear for your feet.
If you are experiencing any discomfort or have any concerns regarding your foot or lower limb, look for our Podiatrists at Straits Podiatry to assist you! Read more if you need help finding the best podiatrist near you in Singapore.
Jackie Tey
Ketua Pakar Kaki, B.Pod (Kepujian). Pakar kaki dan anggota bawah anda bersemangat untuk meningkatkan kesedaran untuk kesihatan kaki dan anggota bawah.
Testimoni Kami
SOALAN LAZIM
Apa itu Podiatry?
Podiatry is an Allied Health field that focuses on the management of lower limb conditions, as well as other aspects of foot care such as prevention, support, and long-term maintenance. It aims to relieve pain, improve mobility, and support daily function. In Singapore, podiatry services are offered across both public hospitals and private clinics, where patients commonly seek help for various foot pain issues, toenail problems, and walking difficulties. Commonly referred to by the public as foot doctors or foot specialists, podiatrists provide non-invasive, conservative care that plays a key role in maintaining long-term lower limb health.
Generally, conditions managed by podiatrists include (but are not limited to):
- Kecederaan sukan
- Sakit kaki
- Sakit tumit
- Kecederaan Buku Lali & Terseliuh
- Fasciitis plantar
- Penyingkiran kuku jari kaki
- Jagung dan calluses
- Kuku kulat
- Kaki rata
- Gerbang tinggi
- Bunions
- Ulser kaki kencing manis
Podiatrists in Singapore are also trained to provide foot health education and prevent injuries from occurring. We can also prescribe custom orthotics or recommend exercises to improve foot and ankle strength.
Mengapa Podiatrist sering dianggap sebagai Doktor Kaki di Singapura?
Podiatrists are commonly referred to as foot doctors in Singapore because we are allied healthcare professionals trained to manage a wide range of lower limb conditions. These include issues involving the bones, joints, muscles, tendons, skin, and toenails that might affect mobility, comfort, or daily function. To support recovery and improve movement, podiatrists might prescribe custom orthotics or recommend other foot care solutions. In Singapore, all practising podiatrists must hold a recognised bachelor’s or doctorate degree in podiatric medicine (DPM) to be qualified to manage these concerns.
Apa itu Podiatri Pediatrik?
Podiatri pediatrik pada dasarnya adalah podiatri untuk kanak-kanak. Ia adalah sub khusus podiatri yang mengkhususkan diri dalam diagnosis dan pengurusan keadaan kaki kanak-kanak. Keadaan kaki kanak-kanak diuruskan sangat berbeza daripada orang dewasa kerana kanak-kanak masih membesar. Pakar podiatrik pediatrik perlu tahu bagaimana untuk mengenal pasti dan membezakan antara perkembangan normal dan tidak normal kanak-kanak.
Keadaan kaki kanak-kanak biasa termasuk (tidak terhad kepada):
- Kanak-kanak kaki rata
- Berjalan kaki
- Berjalan kaki di kaki
- Osteochondroses (contohnya penyakit Sever)
- Mengetuk lutut
Di Straits Podiatry, kami faham bahawa anak anda mungkin berasa gementar ketika menghadiri klinik. Oleh itu, kami mempunyai ruang kanak-kanak yang berdedikasi untuk perkhidmatan podiatri pediatrik yang direka untuk membantu anak anda berasa selesa semasa berunding. Pakar podiatrik pediatrik kami di Singapura sangat berpengalaman dalam keadaan kaki kanak-kanak dan dapat memberikan nasihat pengurusan terbaik untuk anak anda. Kami berhasrat untuk memastikan semua ibu bapa diberi maklumat yang betul dan anak-anak mereka tidak menjalani rawatan yang tidak perlu.
Bilakah Umur Terbaik untuk Membawa Anak Saya Melihat Podiatrist?
There’s no best age to bring your child to see a paediatric podiatrist, as foot conditions can appear at different stages of childhood. For many parents in Singapore, concerns often begin with how their child walks, stands, or whether their foot shape looks quite right. That’s why our paediatric podiatry services range from infancy to adolescence, and our facilities are children-friendly. We have seen infants suffering from ingrown toenails as young as a few days old, which highlights how early certain issues can arise. Overall, if you are concerned about your child’s foot or lower limb structure, walking pattern, or would just like to seek a foot health screening, our paediatric podiatry services are right for you.
Apakah perkhidmatan yang Straits Podiatry sediakan?
Di Straits Podiatry, matlamat kami adalah untuk membantu anda pulih tanpa memerlukan pembedahan. Klinik podiatri kami di Singapura mengkhusus dalam menggunakan teknologi terkini dan terapi canggih untuk melegakan sakit anggota badan anda yang lebih rendah. Satu-satunya "pembedahan" yang kami lakukan di klinik adalah pembedahan kuku jari kaki dan penyingkiran ketuat di Singapura. Walau bagaimanapun, ini adalah invasif minimum, dan anda boleh berjalan keluar dari klinik dengan segera selepas itu.
Senarai perkhidmatan atau rawatan yang kami sediakan termasuk:
- Saringan kaki
- Penilaian biomekanik dan analisis gaya berjalan
- Penjagaan kaki diabetes
- Insole tersuai
- Orthoses kaki buku lali yang disesuaikan
- Ortos pediatrik yang disesuaikan
- Penyingkiran jagung dan kalus
- Rawatan luka
- Penyingkiran ketuat
- Penyingkiran kuku jari kaki
- Terapi gelombang kejutan terfokus
- Terapi gelombang tekanan radial
- Terapi magnetotransduction
Kami adalah salah satu daripada beberapa klinik podiatri di Singapura dengan seluruh pasukan podiatrists dengan pensijilan rawatan gelombang kejutan perubatan. Ini bermakna bahawa kami bukan sahaja klinik yang menyediakan terapi gelombang kejutan, tetapi kami juga mempunyai pengamal yang disahkan di peringkat antarabangsa untuk membantu anda. Kami bangga dalam memastikan bahawa pakar kaki kami di Singapura mempunyai kelayakan terbaik untuk membantu anda.
Bilakah saya perlu melihat seorang Podiatrist?
Podiatrists kami dilatih untuk menguruskan kebanyakan masalah kaki, buku lali dan anggota bawah. Jika anda mengalami ketidakselesaan anggota bawah, sakit atau kesukaran berjalan atau berdiri, adalah dinasihatkan untuk berunding dengan podiatrist. Sekiranya anda masih tidak pasti sama ada kami boleh membantu anda, sila hubungi kami! Kami dengan senang hati akan membantu anda dan menasihati anda dengan sewajarnya.
Apa yang Perlu Saya Bawa untuk Perundingan Podiatri Pertama Saya?
Anda boleh membawa semua laporan perubatan dan senarai ubat anda yang lalu sebelum melihat Podiatrists kami. Ini termasuk sebarang imbasan pengimejan (contohnya x-ray atau MRI) dan laporan bertulis mereka. Ini akan memudahkan kami dalam menyediakan penjagaan holistik terbaik apabila menangani kebimbangan anda. Anda harus membawa kasut anda yang sering dipakai, termasuk kasut sekolah, kasut kerja, dan kasut sukan biasa.
Bagi ibu bapa yang mencari perkhidmatan podiatri untuk anak-anak mereka, anda juga boleh membawa bersama buku kesihatan mereka untuk lawatan pertama. Ini akan membantu kami memahami sejarah kelahiran dan perkembangan anak anda.
Adakah saya memerlukan surat rujukan untuk melihat podiatrist?
Surat rujukan daripada doktor perubatan lain tidak diperlukan untuk berjumpa podiatrist di Singapura. Jika anda mempunyai kebimbangan atau kesakitan anggota bawah, anda boleh menghubungi kami secara langsung untuk menjadualkan temujanji dengan kami.
Walau bagaimanapun, jika anda mempunyai surat rujukan daripada mana-mana doktor perubatan atau pengamal am untuk berjumpa pakar kaki di Singapura, anda harus membawa mereka bersama untuk temu janji anda. Ini secara amnya akan membantu kami memahami keadaan perubatan anda dengan lebih baik. Ia juga boleh membantu anda mendapatkan bayaran balik jika insurans anda memerlukan surat rujukan untuk berjumpa doktor kaki atau pakar kaki.
Di Straits Podiatry, kami menerima rujukan daripada mana-mana doktor perubatan atau pengamal am untuk pelbagai keadaan anggota bawah. Sekiranya polisi insurans anda di Singapura memerlukan surat rujukan untuk podiatri, sila rujuk mana-mana Pengamal Am Perubatan Healthway untuk mendapatkan bantuan!
Bagaimanakah saya boleh membuat temujanji?
Menempah janji temu dengan kami adalah mudah! Anda boleh memilih kaedah berikut:
Klinik kami dibuka dari Isnin hingga Sabtu, 9 pagi hingga 5 petang, tidak termasuk cuti umum. Pertanyaan anda adalah penting kepada kami dan kakitangan klinik kami akan bertindak balas sebaik sahaja mereka kembali ke pejabat semasa waktu operasi. Jika tidak, platform tempahan dalam talian kami tersedia 24 jam, jadi jangan ragu untuk membuat tempahan dan anda akan menerima pengesahan selepas itu.
Lokasi klinik kami
3 Klinik Podiatri
Terletak beberapa minit dari stesen MRT
Buona Vista
Terletak di sebelah Rochester Mall
Alamat Klinik:
31 Rochester Dr, #02-01 (Blok Hotel), Singapura 138637
Stesen MRT terdekat:
Buona Vista ((CC22 / EW21) )
Waktu Operasi:
Isnin hingga Sabtu: 9 pagi hingga 6 petang
Ditutup pada cuti umum
Telefon:
(+65) 6990 4574
Katong
Terletak di i12 Katong
Alamat Klinik:
i12 Katong, Kolektif Teras
112 Pantai Timur Rd, #03-01/02/03/04/28, Singapura 428802
Stesen MRT terdekat:
Perarakan Marin (TE26)
Operating Hours:
Monday to Saturday: 9 a.m. to 6 p.m.
Closed on Wednesday & Public Holidays
Telefon:
(+65) 6990 4574
Orchard
Terletak di The Centrepoint
Alamat Klinik:
Perubatan Jepun Healthway
@ Pusat
176 Jalan Orchard,
#06-05,
Singapura 238843
Stesen MRT terdekat:
Somerset (NS23)
Operating Hours:
Monday to Saturday: 9 a.m. to 6 p.m.
Closed on Wednesday & Public Holidays
Telefon:
(+65) 6990 4574
Buona Vista
Terletak di sebelah Rochester Mall
Alamat Klinik:
31 Rochester Dr, #02-01 (Blok Hotel), Singapura 138637
Stesen MRT terdekat:
Buona Vista (CC22 / EW21)
Waktu Operasi:
Isnin hingga Sabtu: 9 pagi hingga 6 petang
Ditutup pada cuti umum
Telefon:
(+65) 6990 4574
Katong
Terletak di i12 Katong
Alamat Klinik:
i12 Katong, Kolektif Teras
112 Pantai Timur Rd, #03-01/02/03/04/28, Singapura 428802
Stesen MRT terdekat:
Perarakan Marin (TE26)
Operating Hours:
Monday to Saturday: 9 a.m. to 6 p.m.
Closed on Wednesday & public holidays
Telefon:
(+65) 6990 4574
Orchard
Terletak di The Centrepoint
Alamat Klinik:
Perubatan Jepun Healthway
@ Pusat
176 Jalan Orchard,
#06-05,
Singapura 238843
Stesen MRT terdekat:
Somerset (NS23)
Operating Hours:
Monday to Saturday: 9 a.m. to 6 p.m.
Closed on Wednesday & public holidays
Telefon:
(+65) 6990 4574